January 29, 2026
post
10 Key Takeaways from IMSH
What We Learned About the Future of Healthcare Simulation Each year, IMSH brings together top leaders from healthcare education and training. From educational sessions to research presentations, panel discussions, and workshops – we did it all this year! During the course of our time at this year’s conference, we gathered information and compiled our top…

What We Learned About the Future of Healthcare Simulation
Each year, IMSH brings together top leaders from healthcare education and training. From educational sessions to research presentations, panel discussions, and workshops – we did it all this year!
During the course of our time at this year’s conference, we gathered information and compiled our top ten takeaways from the event to share with other healthcare educators and trainers looking for important themes coming out of IMSH.
What We Heard in Educational Sessions
1. Communication is key
A theme we heard again and again – from educators, leadership, clinicians – communication is not only key, it’s critical.
We also heard that while it’s a primary focus across both academia and healthcare settings, it is one of the most difficult skills to replicate for simulation and provide meaningful, psychologically safe learning experiences.
Communication is not simply bedside manner. It’s much bigger than that and involves succinctly providing key information to interprofessional team members, educating patients and family members, and it is one of the first building blocks to an effective therapeutic relationship.
With the advancement of artificial intelligence (AI), learners now have opportunities to talk to their virtual patients, asking questions for motivational interviewing or practicing skills to de-escalate a tense situation.
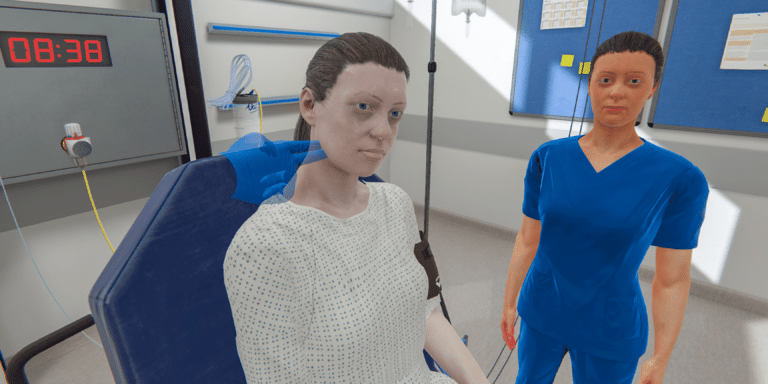
VR simulations, like those from OMS, provide a unique space for learners to practice independently, working through the difficulties and challenges of learning how to effectively communicate within the healthcare setting.
This is likely to continue to grow, as the need for tools that directly contribute to communication skills are highly in demand.
2. Artificial Intelligence in simulation
Another hot topic during IMSH was the use of AI in healthcare simulation – it’s a topic we know well, given our Clinical Product Manager, Dawn-Marie Dunbar, RN, MSN/Ed., CNE, CHSE, gave a presentation on it during SimGhosts. We turned that into a webinar, if you’d like to watch that here.
Many questions and concerns remain about how to implement and use AI – it seems the consensus here is that while AI requires careful consideration, it is here to stay, and we ought to embrace it with sound ethics and intention.
Interestingly, we often heard about AI prompting, to develop cases or assist in administrative tasks. While certainly an area of importance, we didn’t hear much about AI use in simulation, and how that can enhance presence, immersion, and reality for learners.
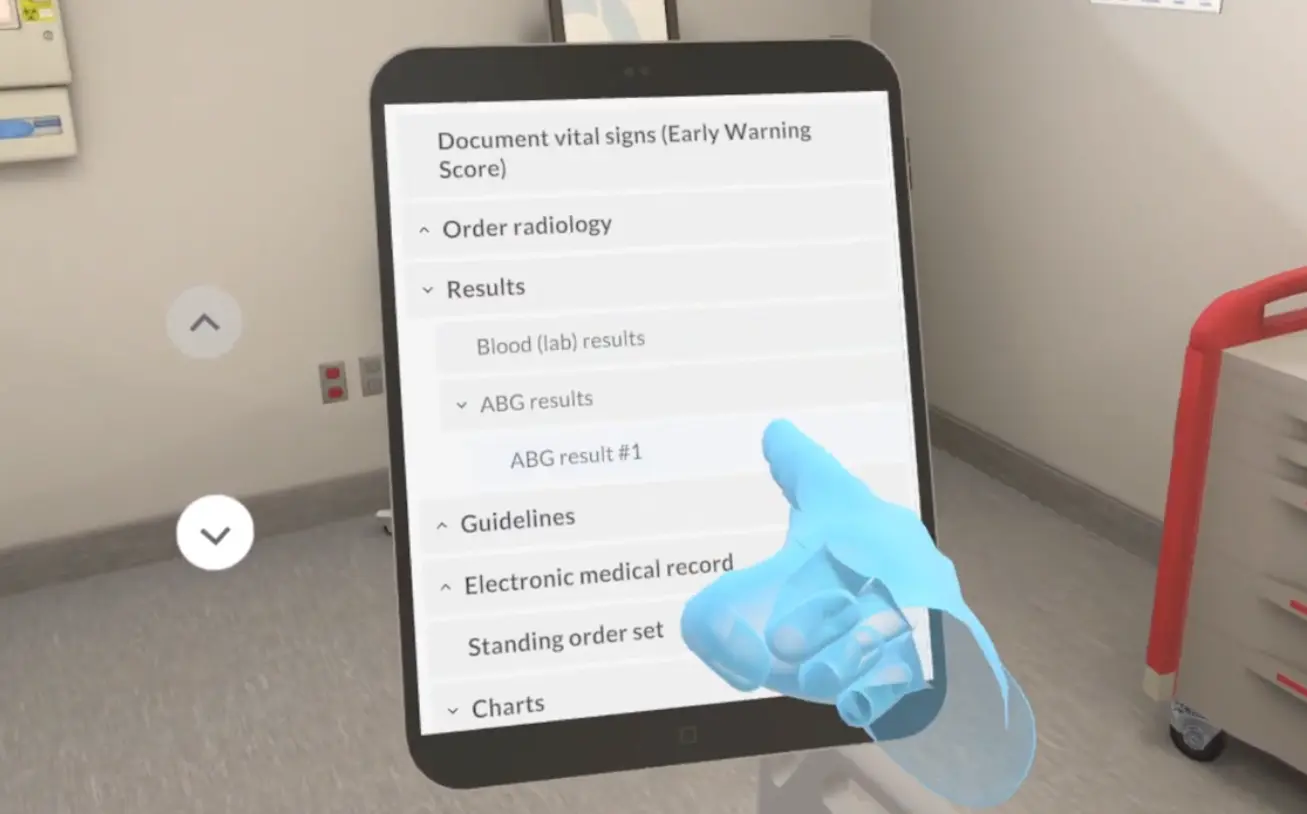
AI has already been a part of OMS scenarios, particularly for adaptive simulations that show a patient’s physiology change based on the learner’s actions.
However, there’s another use of AI here – as mentioned above, AI supports the use of your voice and frees up the need for menu-based controls. This creates a much more open and realistic simulation, often best for more advanced learners, which replicates the entirety of the clinical interaction, not just its parts.
The advancement of AI within the OMS platform creates an open and engaging virtual environment that supports natural interactions reflective of clinical practice. Learners can interact, pick up, and place objects to support procedural skills or practice speaking with virtual patients, families, and team members to support patient-centered care and therapeutic communication.
The use of AI will continue to expand, particularly in supporting scalability of simulation, helping learners everywhere gain equitable access to healthcare simulation.
3. Obtaining buy in
Often, we heard budget come up as a main barrier for educators seeking to implement new tools into their programs to support learners.
Some of the most packed sessions we attended were on demonstrating the value of these tools and making the case to leadership for support.
One of the key takeaways we gathered from these sessions was the importance of engaging with leadership directly, and aligning the intended use or expected outcomes to their goals is key. For example, inviting leadership to experience a VR simulation in-person can go a long way toward understanding the value and securing financial support.
Another suggestion was tracking your “turnaways.” How many simulation requests from constituent departments do you turn down due to capacity constraints? What are the consequences of that loss of training experience?
This approach gets everyone on the same page while demonstrating the value of the tool before investing or committing to its use.
We expect this to continue to be a common challenge across academia and healthcare systems, as the demand for simulation and scalability continues to increase.
What Customers Told Us Directly
4. Psychological safety in VR
One of the main benefits highlighted from virtual reality simulations was the inherent psychological safety of the platform.
One customer told us “it’s the ultimate psychological safety” – learners navigate the simulation independently, are able to make mistakes, and receive immediate feedback. They can then repeat the scenario and, later, debrief with a small group.
Learners from multiple institutions have highlighted the autonomous practice they get from running the simulation – this is particularly relevant for students, given that leading a patient case, even with minimal supervision, is an opportunity that students rarely receive in clinicals.
For educators interested in finding a tool to support learners in meaningful ways, VR provides a psychologically safe space for learners, which we’ve heard repeatedly from direct conversations with customers and learners, as well.
5. Importance of cross-departmental collaboration and rollout support, implementation
Collaboration – it’s a cornerstone to patient care. In speaking with our customers, it’s also crucial to the effective, smooth implementation of a tool like VR.
Many of our customers stressed the importance of bringing in other departments early on in the process. For example, bringing in IT to determine feasibility, flag technical concerns, and support the rollout can make all the difference.
Finding support from colleagues across departments invites further discussion from points of view that differ, creating a more comprehensive map for a rollout.
This also applies to fellow educators and folks who will be teaching learners the technology. Many customers mentioned creating a day or block of time to bring educators in before learners, to get familiar with the technology, see its potential, and ideate how best to implement.
Collaborating across departments was a key component to the success of many customers’ implementation experiences, and is one that was highlighted to us again and again about just how imperative it is to develop an implementation team to support your process.
6. Supporting the transition to practice
For many, the transition to practice was top of mind – between the educators preparing students for their first year of practice to the clinicians supervising, supporting, and mentoring them.
We know that the transition to practice is often a difficult period, and there were several ways that customers spoke about how healthcare education and training can provide further support.
One of the most-discussed methods for support was to connect the academic institution and clinical partners to collaborate on how educators can better prepare students while healthcare systems can better support their transition to practice.
Often, we heard about the use of tools, like VR, to help students bridge any gaps in knowledge or experience a clinical situation they did not see during their rotations.
Some students have reported that VR has bolstered their confidence and has directly helped them answer questions on their licensure exam.
VR scenarios can also be used during the transition to practice to support onboarding, align new hires to institutional policies and procedures, and can be used in part as an assessment tool to evaluate clinical readiness and ensure safe practices.
Based on our customers’ reports, we expect this topic to continue to be a discussion at the forefront, and we also anticipate we’ll be seeing more use of tools like VR to support the process alongside structured debriefs and support from educators.

What We Observed from Prospects & the Market
7. Intentionality with purchasing digital tools
When seeking to use new tools, there can be so much information to take in that we can get a bit lost – that’s why it’s imperative to determine the intended use and outcomes of the tool prior to starting the search.
Many customers noted growing momentum toward the adoption of digital tools to support learning and recommended starting with learning objectives, concepts, or key takeaways that educators are looking to gain for their learners.
This provides a guide and map from which you can work to ensure that the digital tool you select actually aligns to the goals you’re setting.
Customers stressed the importance of selecting VR scenarios with intention, not using VR for VR’s sake.
They also addressed the importance of communicating this thought process to learners to make it clear why they’re doing this now and what they should expect to learn from it.
8. Modalities
How should you incorporate tools like VR into coursework and debriefing?
We heard this a lot – there are so many different ways you can use a tool like VR. In the classroom, you can bring clinical concepts to life, have learners work through a simulation in small groups, or assign work independently to learners.
Regardless of where VR appears in your program, it’s imperative that it be aligned within a structured approach and with faculty who are both trained on the technology and in the debriefing.
An interesting takeaway we heard from several customers was to consider a small adjustment to the debrief process. Some allot more time to process post-simulation while others have started to incorporate a technical debrief at the beginning.
This allows learners to process their experience with the technology first, and once they’ve had the opportunity to talk through that, educators continue with a structured debrief.
9. Meaningful learning
The learner experience is highly important and is something to carefully consider when implementing a new tool to support learning.
It must be relevant and useful to learners while providing a meaningful experience supports readiness.
With tools like VR, immersion and autonomy support this meaningful learning experience, ensuring learners are ready to bridge the gap between theory and clinical practice, with virtual patients who are representative of the situations that many clinicians will encounter over the course of their practice.
The Big Pattern That Ties It All Together
10. Clinical readiness and competency-based education are the new ready.
Students become clinically ready as they move through a competency-based education framework, with meaningful learning experiences along the path.
Learners at healthcare systems, for instance, also require meaningful learning experiences, and in addition, the need for standardized processes is paramount, particularly across multi-site organizations.
Tools like VR support these individual learning experiences, creating both a standardized and personalized experience, helping to elevate learners, empower educators, and transform outcomes.
To learn more about how OMS supports clinical readiness, set up a time to speak with one of our Educational Specialists here.
Related
Ready to get real?
See how OMS can help your organization build confidence, competence, and clinical readiness for today’s healthcare.