Deliver simulation at scale with Oxford Medical Simulation
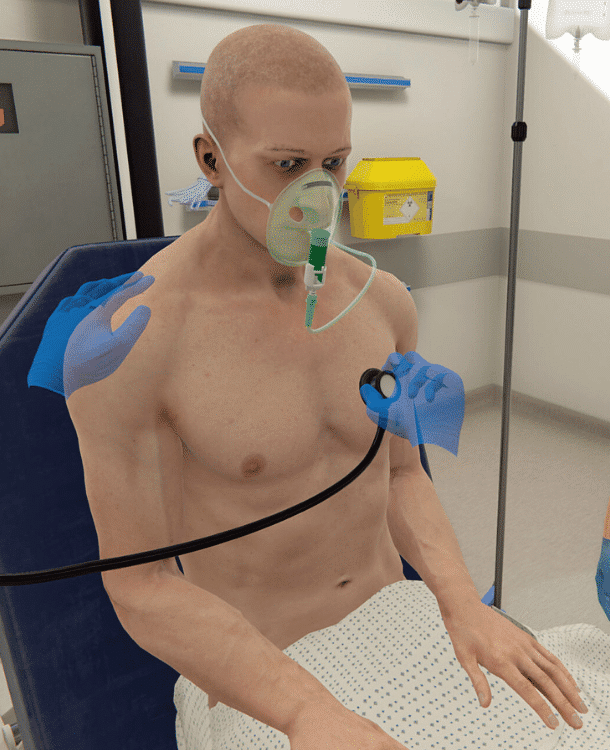
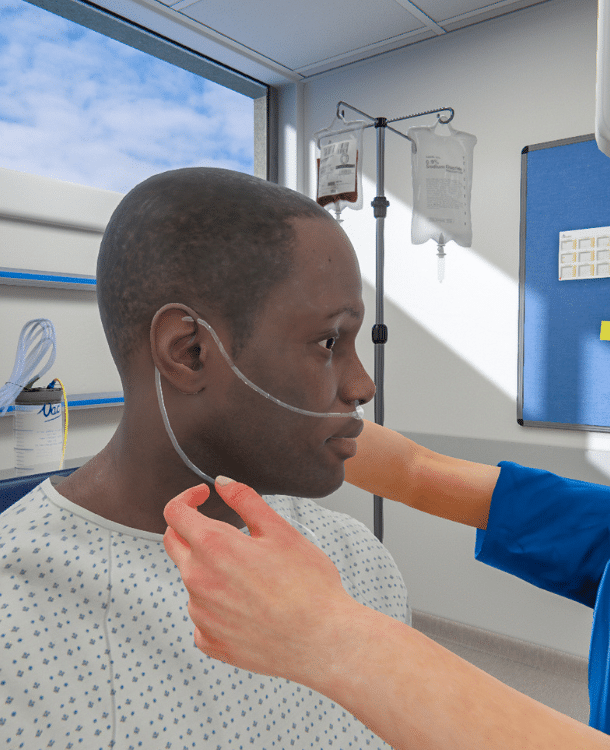
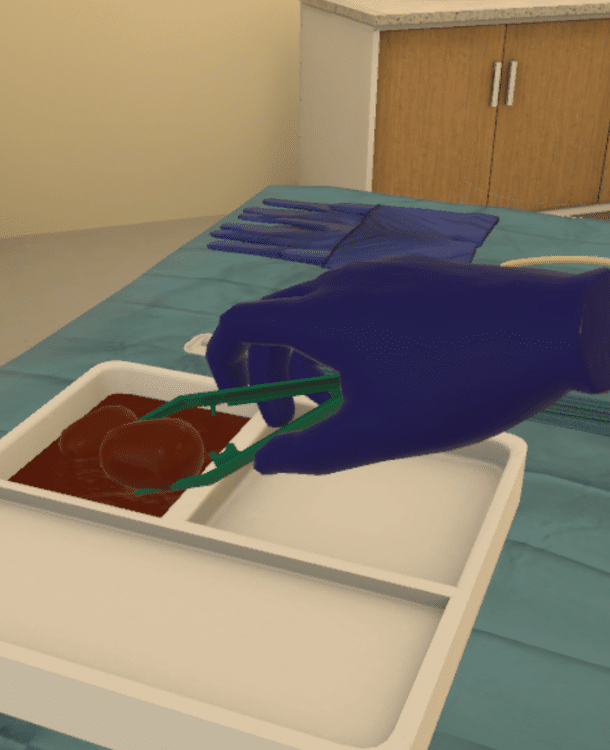
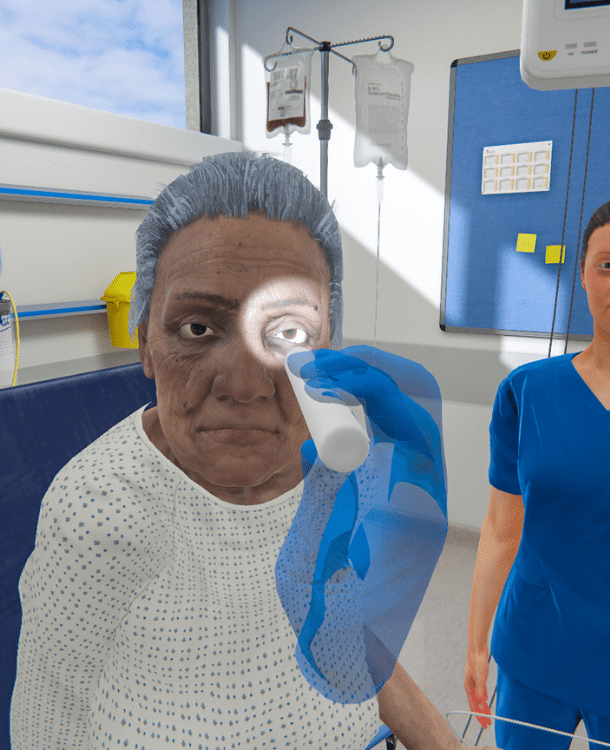
Combining healthcare education and competency assessment with dynamic VR simulations
Created by experts,
backed by evidence
A powerful learning platform bridging theory with immersive scenarios - offering in-depth insights into clinical performance
Practice anytime, anywhere
On the unit, in the classroom, or at home – OMS you can take anywhere.
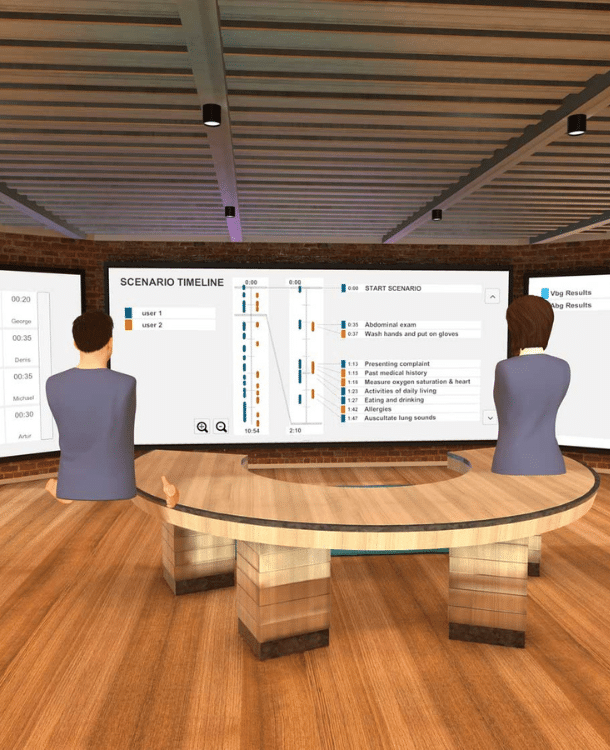
Self-directed and facilitated
Practice solo for self-paced learning or with expert educators and your team to maximize collaboration.

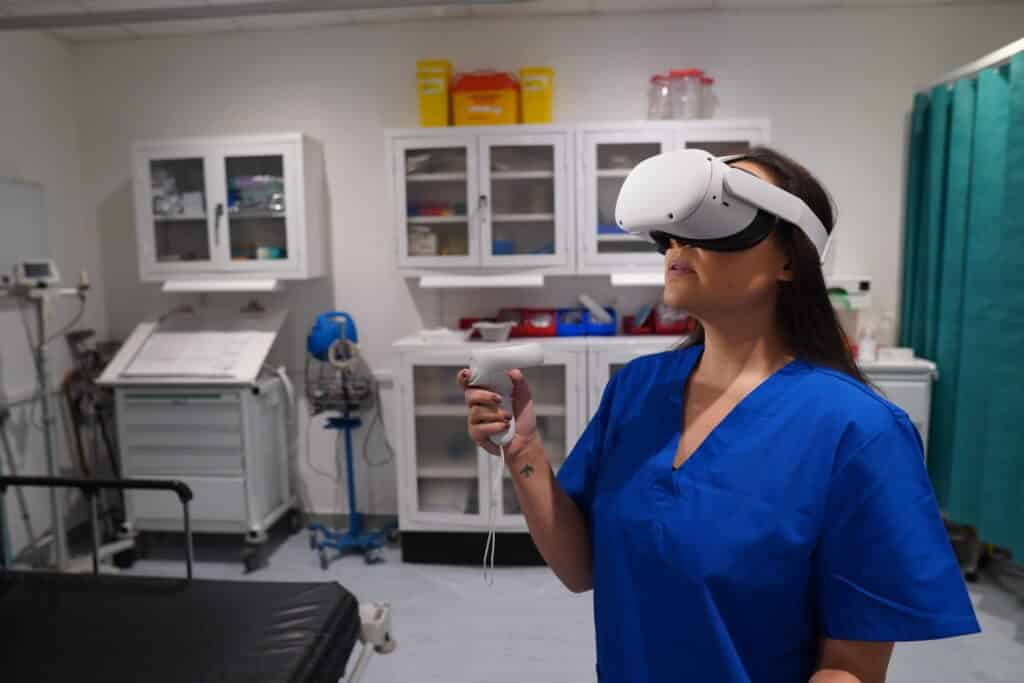
In VR and on screen
Use virtual reality headsets for ultimate immersion, or deliver on screen to ensure accessibility at scale.

Adaptive and standardized
Provide dynamic clinical experiences on-demand, with objective measures of competence to optimize performance.
Practice anytime, anywhere
On the unit, in the classroom, or at home – OMS you can take anywhere.
Self-directed and facilitated
Practice solo for self-paced learning or with expert educators and your team to maximize collaboration.

In VR and on screen
Use virtual reality headsets for ultimate immersion, or deliver on screen to ensure accessibility at scale.

Adaptive and standardized
Provide dynamic clinical experiences on-demand, with objective measures of competence to optimize performance.
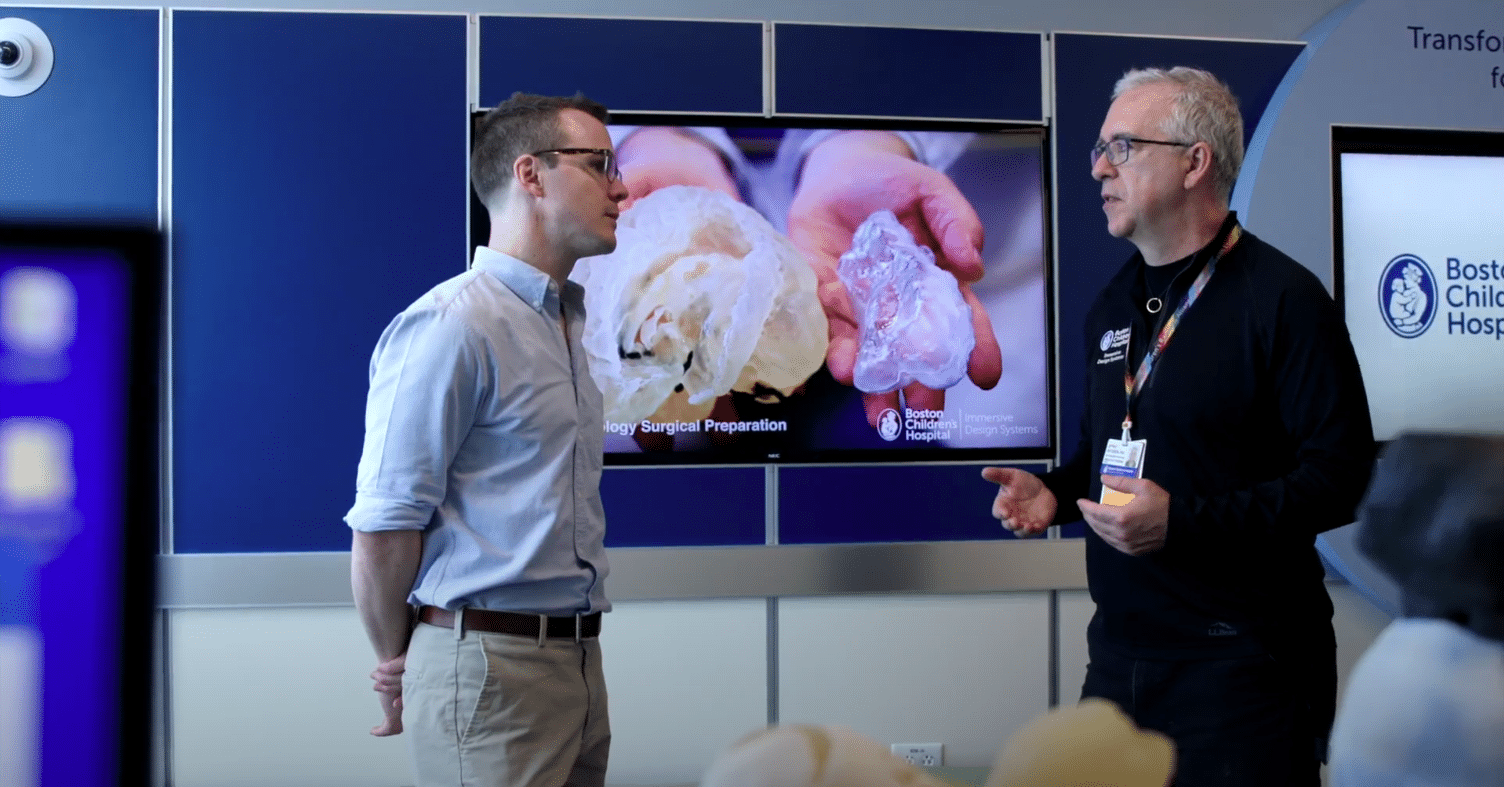
Our trusted partners
World-leading institutions use OMS to scale clinical education, training, and assessment across nursing, medicine, and allied health.

Why OMS?
Depth, breadth, data, and expertise combine to deliver simulation and competency assessment at scale.
Tailored learning solutions
Diverse methods of engagement to support learners in any situation
Build skills, reduce costs
Prepare learners for practice while reducing time, effort, and equipment costs.
OMS in Healthcare Systems
Our platform helps systems:
- Recruit
- Onboard
- Train & assess
- Upskill & reskill
- Support & retain
- Reduce costs
OMS in Academic Institutions
Our platform helps institutions:
- Scale clinical placements
- Map & track competency
- Standardize feedback
- Eliminate bias in assessment
- Reduce pressure on faculty
- Reduce costs