It's amazing. You feel like you're in a whole other world!
Melissa Boggan, Nursing Student
Johns Hopkins University (JHU) School of Nursing is one of the world’s leading nursing programs, driving advancements in education, research, and practice.
As their simulation program expanded, the team at JHU were looking to scale delivery of simulation quickly, using the leading technology and software available. They therefore implemented Oxford Medical Simulation (OMS) Virtual Reality scenarios in pre-licensure and advanced practice programs across the nursing school.
The newly implemented VR program is part of their integrated simulation training program, including manikins and live actors, and complements clinical visits with hospital patients.
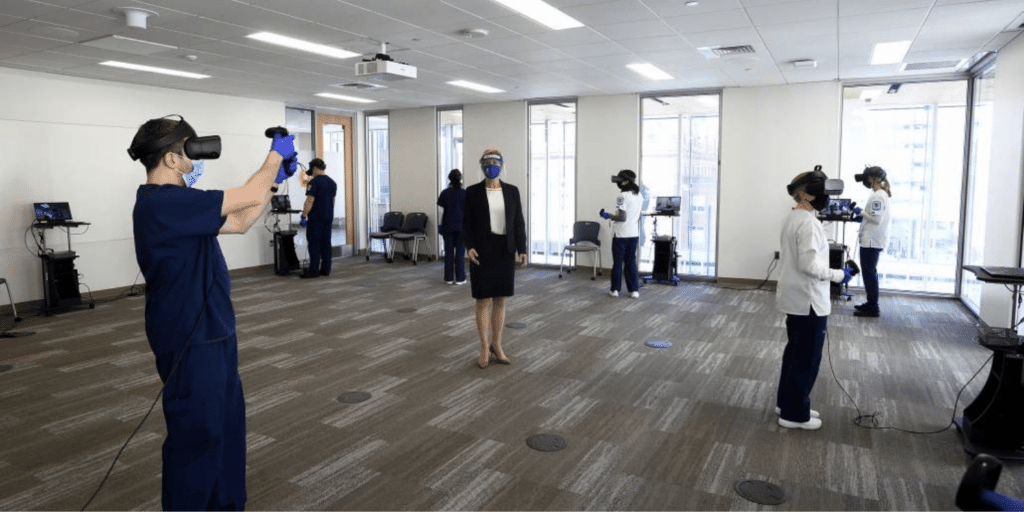
JHU’s Virtual Reality lab provides fully immersive virtual placements for multiple nursing programs, including the newly launched DNP Nurse Anesthesia and DNP Pediatric Dual Primary/Acute Care Nurse Practitioner programs. The program’s implementation in 2020 helped JHU maintain training momentum during the COVID-19 pandemic.
“We rolled out the [OMS] virtual simulation platform over the summer, during COVID, and were able to train about 400 students in a short time frame,” says Kristen Brown, advanced practice simulation coordinator at the School of Nursing.

VR simulation, a growing movement in nurse training before the pandemic, took on new meaning when restrictions impacted learning. VR simulation made socially distanced simulation possible. The spread of coronavirus “put steam behind moving the project forward,” says Nancy Sullivan, clinical simulation director at the school.
Implementing VR in practice
“Since March and the beginning of restrictions for in-person clinical experiences, traditional clinical and simulation for MSN (Entry Into Nursing) students were conducted virtually to enhance and sometimes replace clinical hours. Virtual or remote simulation also replaced non-direct clinical hours for advanced practice DNP students.”
Maximizing experiential learning opportunities, JHU learners begin with the scenarios on-screen. Students who score 80% and above can visit the school’s brand-new Virtual Reality Lab, where COVID-19 safety protocols enable them to use the VR headsets for a fully immersive experience.
Whether on-screen or via VR headset, each OMS scenario places the learners in a virtual setting with a nursing assistant, who helps users assess and manage their virtual patients. With adaptive conversation, dynamic physiology, and powered by artificial intelligence, OMS virtual patients enable patient avatars to alter their behavior based on the learner’s interventions. “Depending on when you do something, the physiological response of the patient changes,” Brown explains. “When I put the oxygen on, or how much oxygen I give, changes the scenario. It adjusts to the learner.”
“I first used the on-screen version last semester,” recalls Kristin White, a pre-licensure student who graduates from the Entry into Nursing Practice program in May. “It was an asthma patient. We practiced at home and had to score 80% on different tasks. Then we got to do it with the headset on campus, which was great, almost like real life.”
Another nursing student, Melissa Boggan, says, “It’s amazing. You feel like you’re in a whole other world.”
Following Virtual Reality sessions, students gather, at a safe distance, with their instructors to participate in a group debrief session. Together with their instructors, students discuss the case, review their performance, ask questions, learn as a team, and become better prepared for clinical practice.
Students then repeat scenarios to help improve their performance and reduce the emotional stressors that can derail procedures. “And they don’t run the risk of hurting anyone,” Brown says. “They learn critical thinking skills while being exposed to high-risk situations not seen very often. It’s great preparation.”
Benefits of VR in Nursing Education
Virtual Simulation has numerous benefits for nursing students:
- Increasing experiential learning opportunities
- Improving performance and reducing emotional stressors through repetition
- Better preparing new nurses to enter the workforce
- Ultimately protecting patients and improving patient care

VR simulation, as a tool in the sim toolbox, has extensive benefits for the nursing profession. “It has implications on enrollment and increased delivery of online programs, allowing nurses to remain in the workforce while advancing education,” Brown says. “More education rooted in experiential learning will produce a better-prepared workforce improving patient care.”
Brown and Sullivan are also researching how VR compares with other simulation methods and clinical practice. Early results are positive, with user ratings being “very high in terms of usability and the scenario debriefing.”
Vitally, when students compare OMS VR scenarios to traditional simulation and clinical experience, they either rated OMS “‘’similar’ or ‘higher'” illustrating the quality of the VR experience relative to traditional approaches.
The JHU simulation team is now expanding OMS use in their virtual simulation program, continuing to provide world-leading simulation opportunities to their students.
