Scalable. Flexible. Versatile.
Meet your learners where they are.
Engage your learners with immersive VR simulations in-headset or on-screen, promote professional development, and set the standard for patient care.
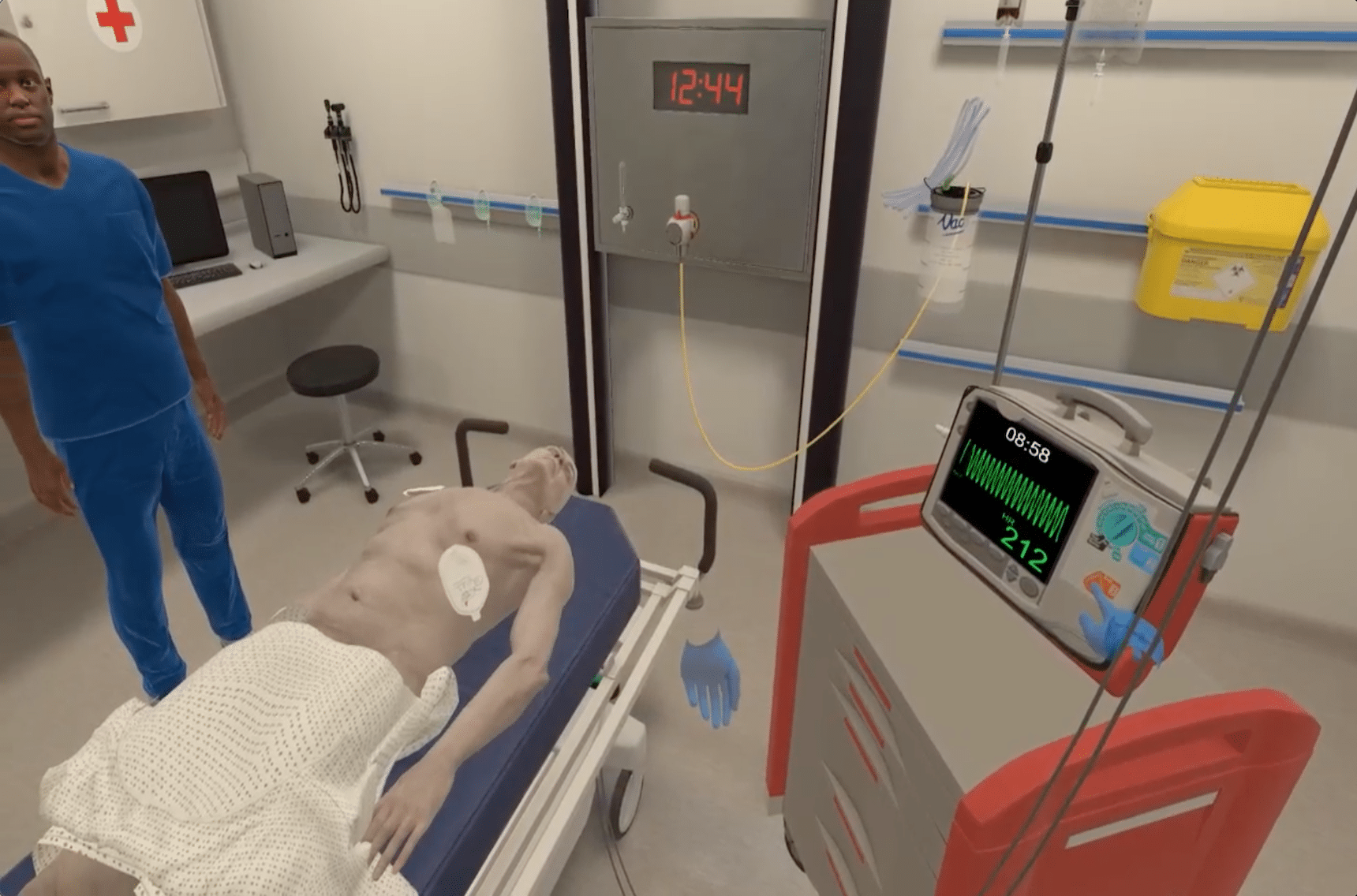
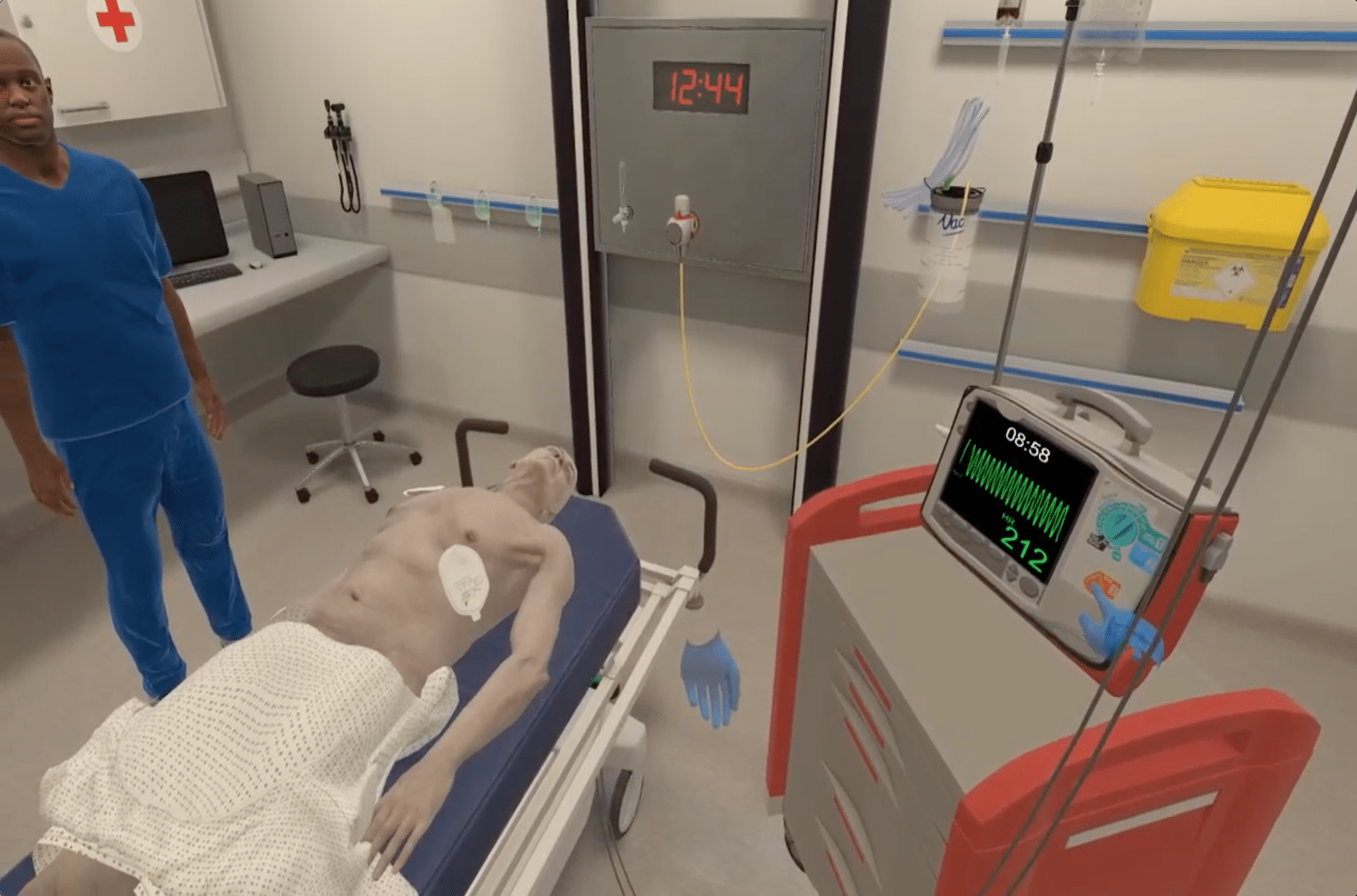
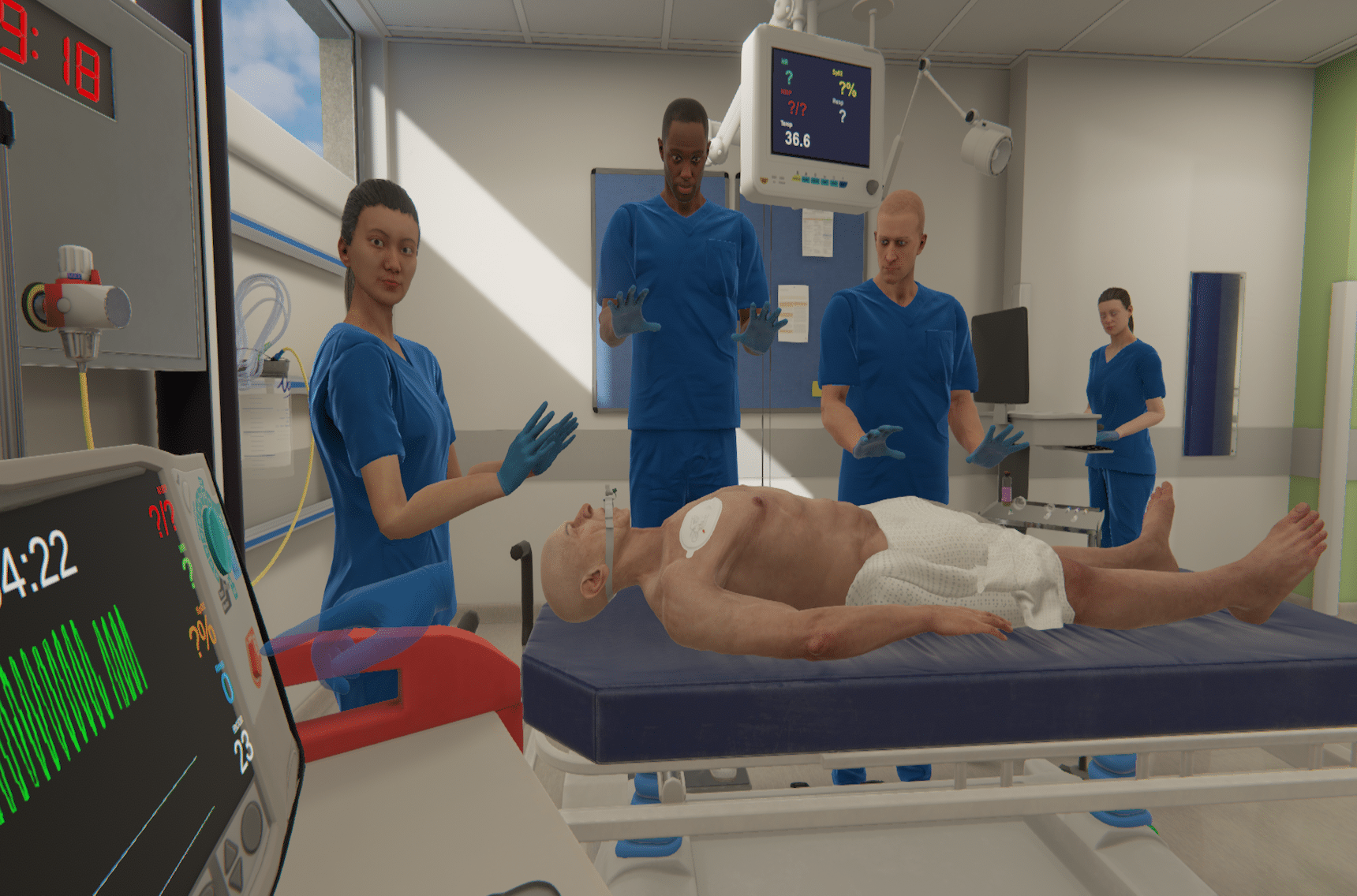
The room? Virtual. The care? Real.
Build skills with the best of both worlds - we've got you covered with every modality you need to match any objective you have.
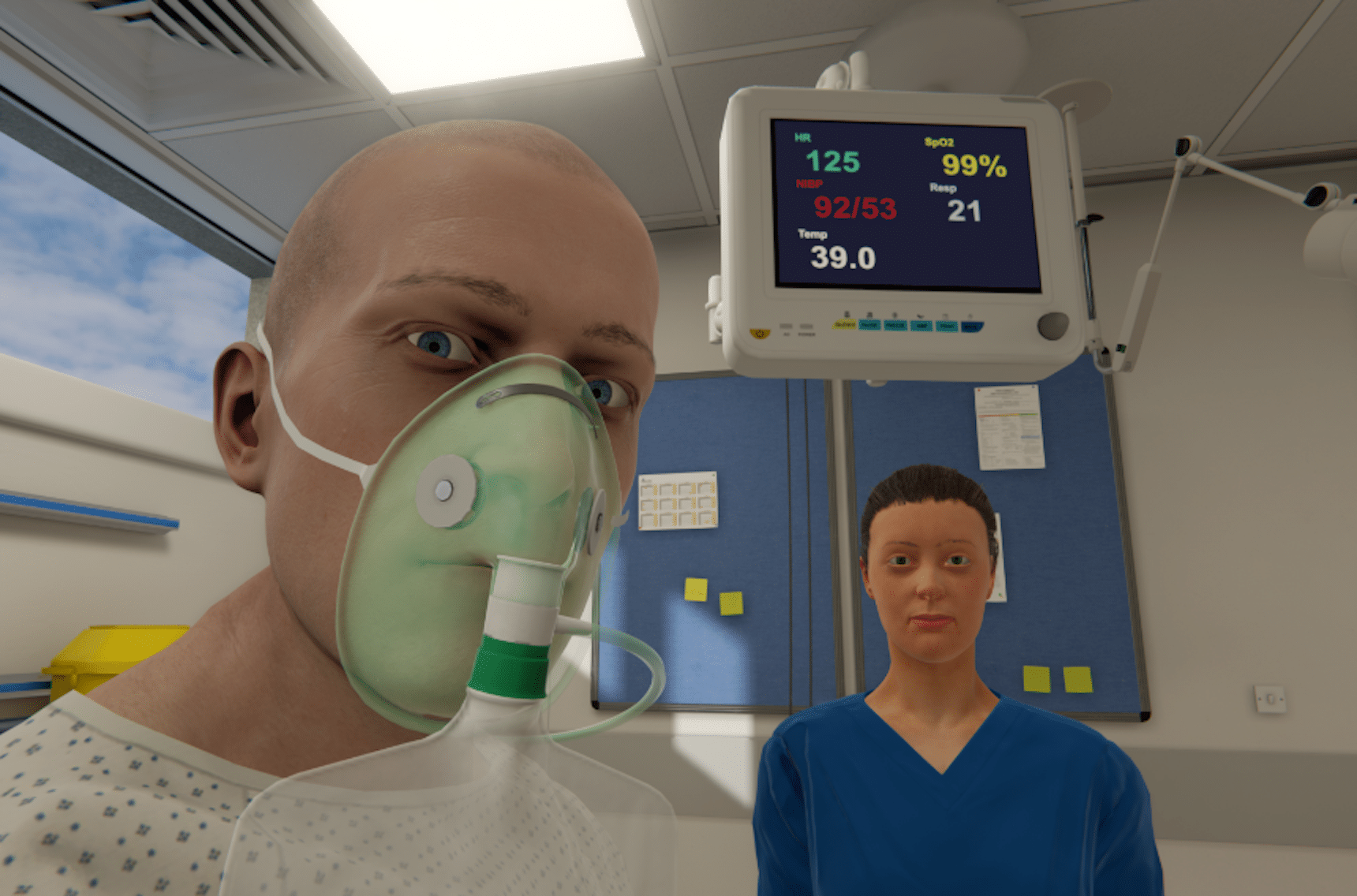
Single-user Training
Transfer knowledge to practice in-headset or on-screen.
Utilize flexible, accessible, and repeatable simulations that emphasize clinical reasoning and decision-making skills.
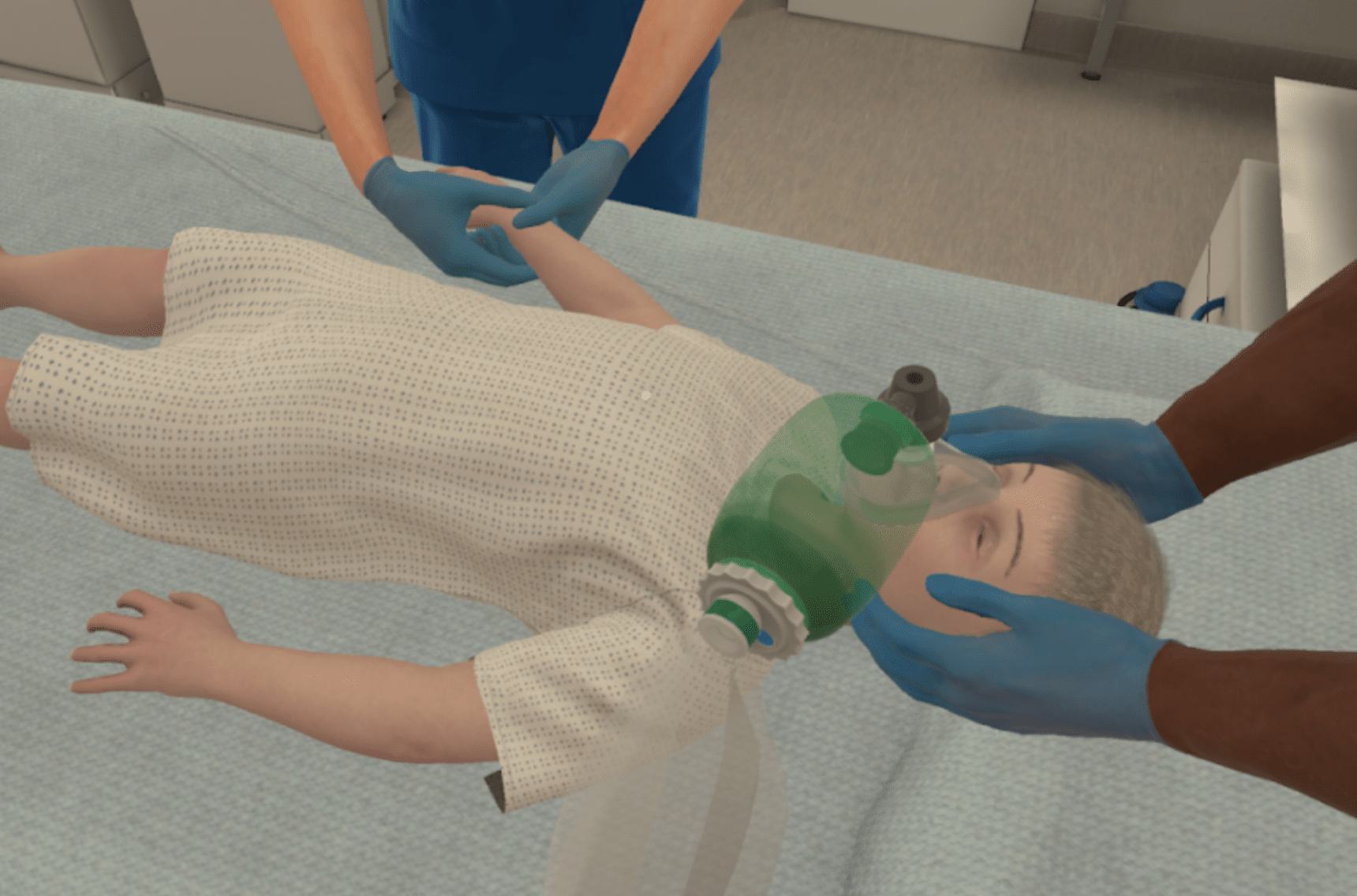
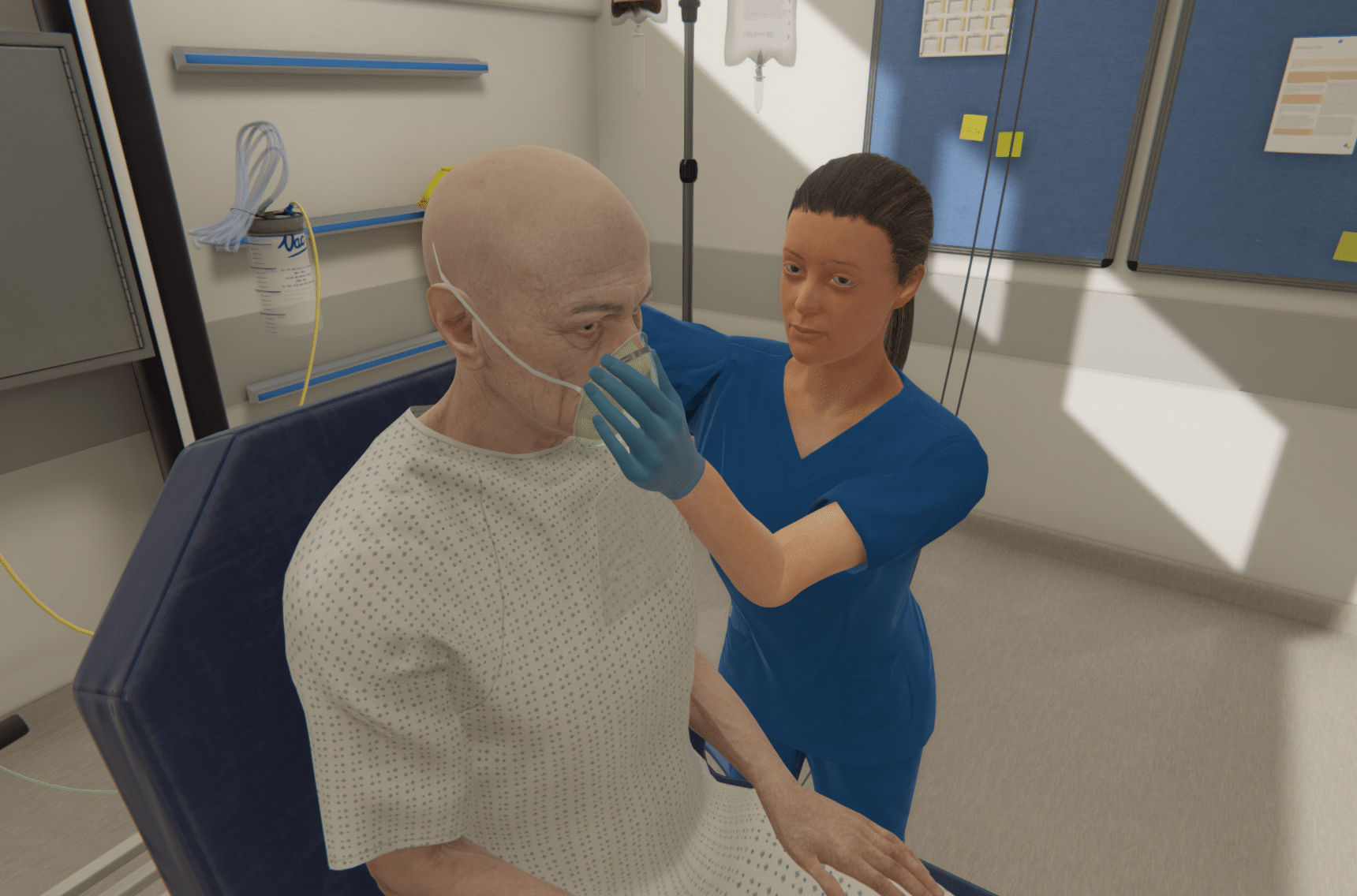
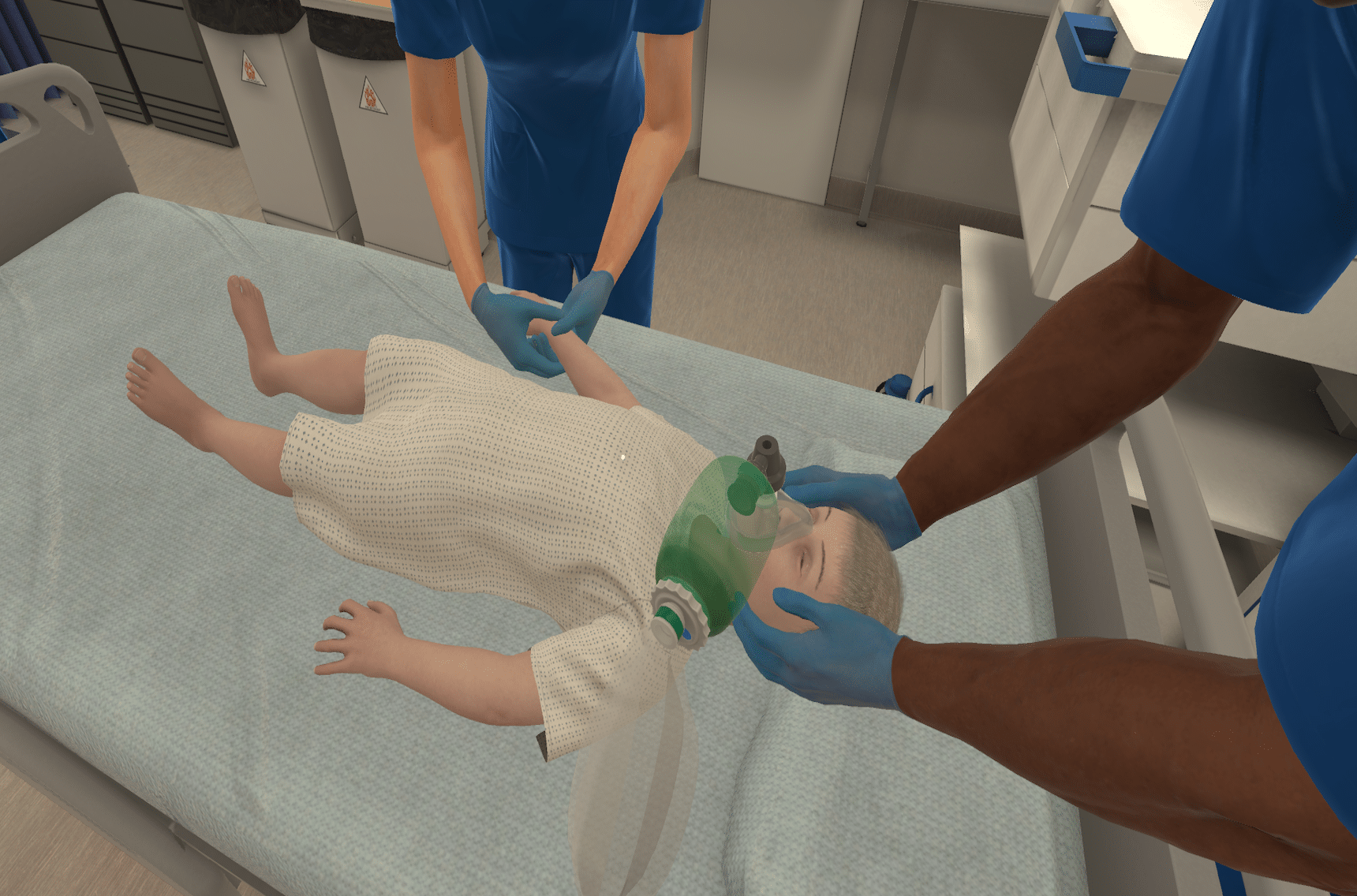
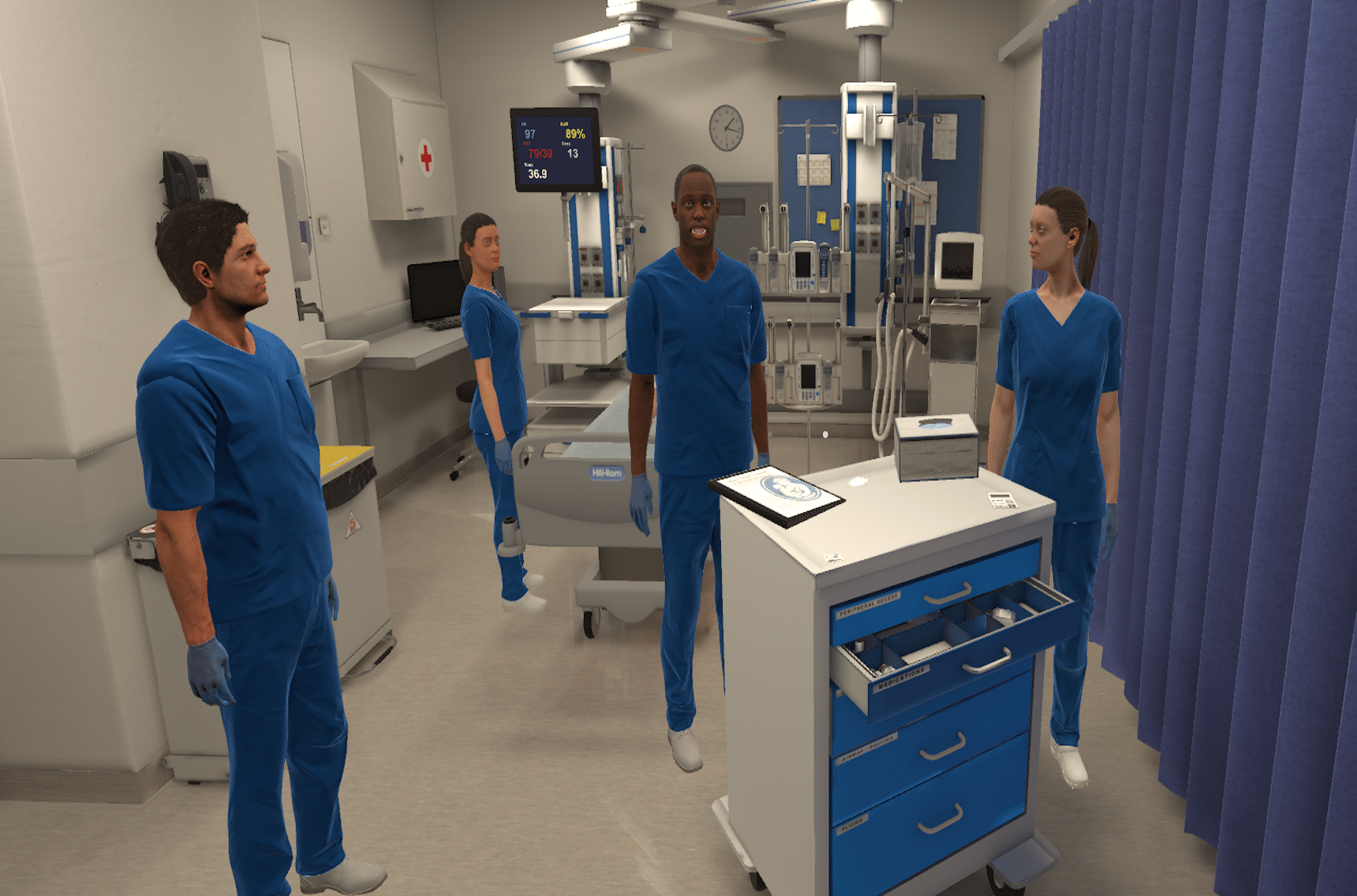
Multi-user Training
Collaborate across disciplines.
Work in interprofessional teams to collectively develop and implement timely treatment interventions. Debrief as a group and receive team-based feedback for a comprehensive view of clinical performance.
Multiparticipant training
Collaborate across disciplines
Work in interprofessional teams to collectively develop and implement timely treatment interventions. Debrief as a group and receive team-based feedback for a comprehensive view of clinical performance.

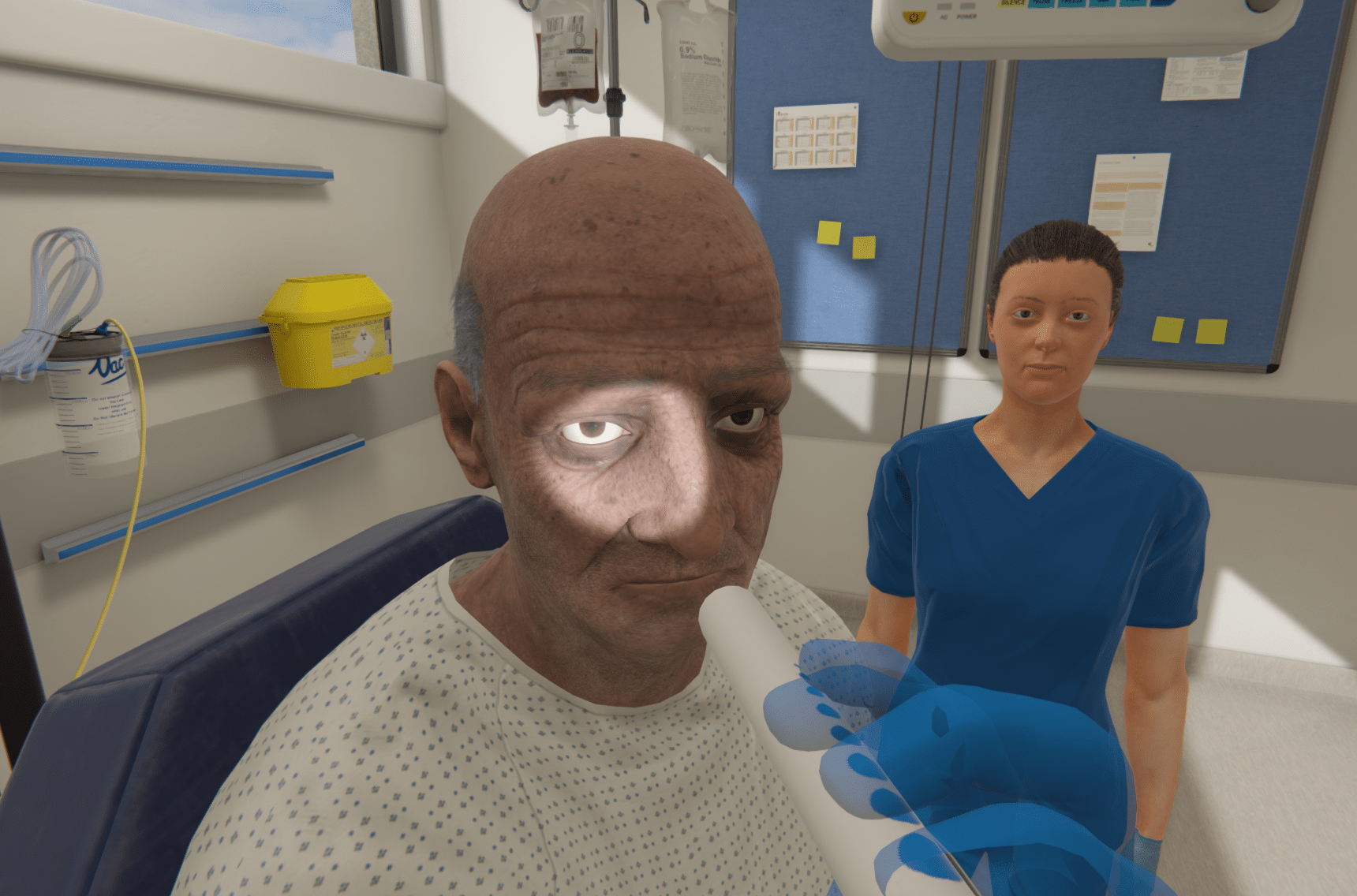
Multi-patient
Master prioritization, delegation, and task-switching.
Prepare for the transition to practice, applying complex clinical decision-making skills in scaffolding scenarios.
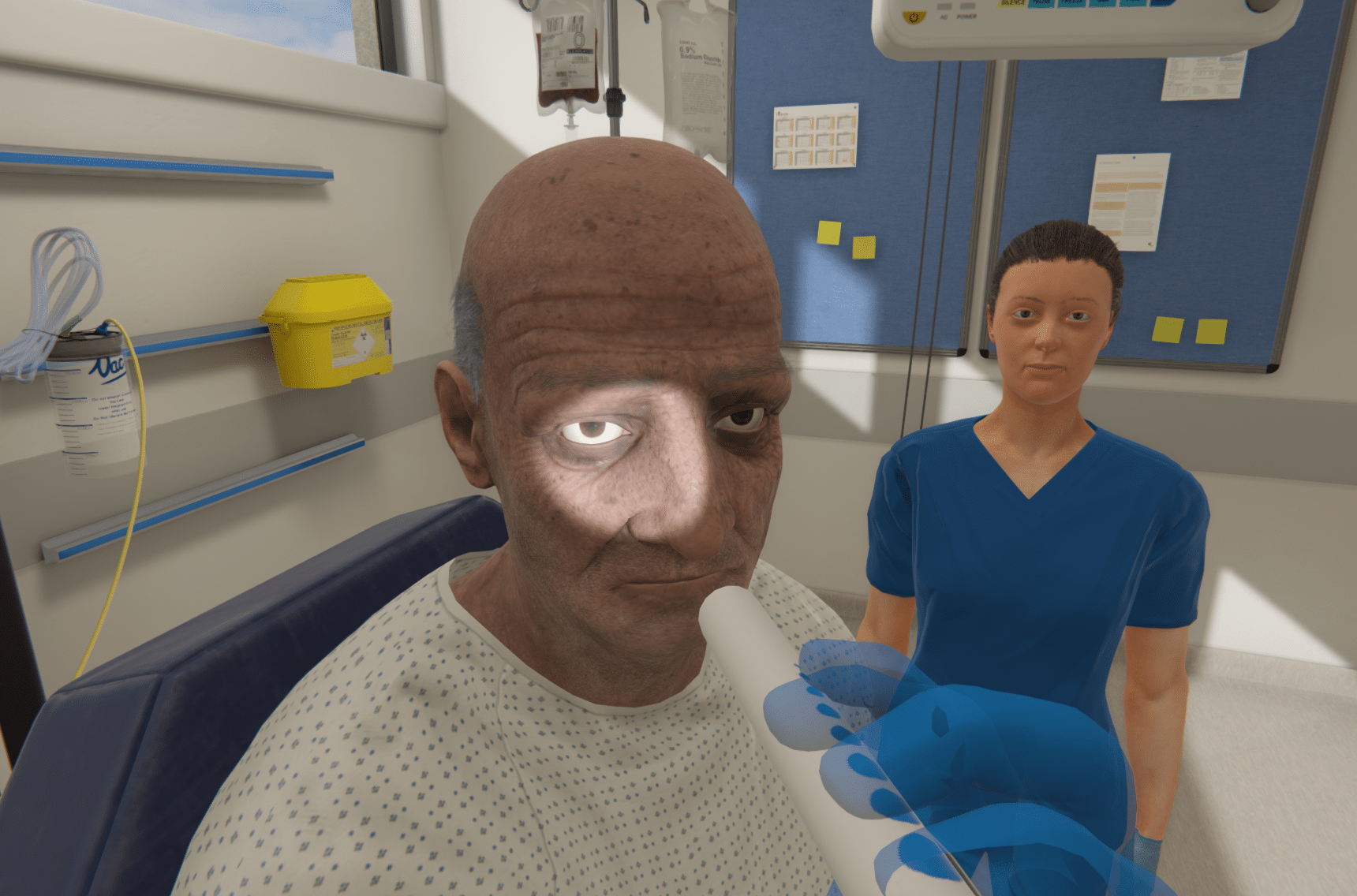
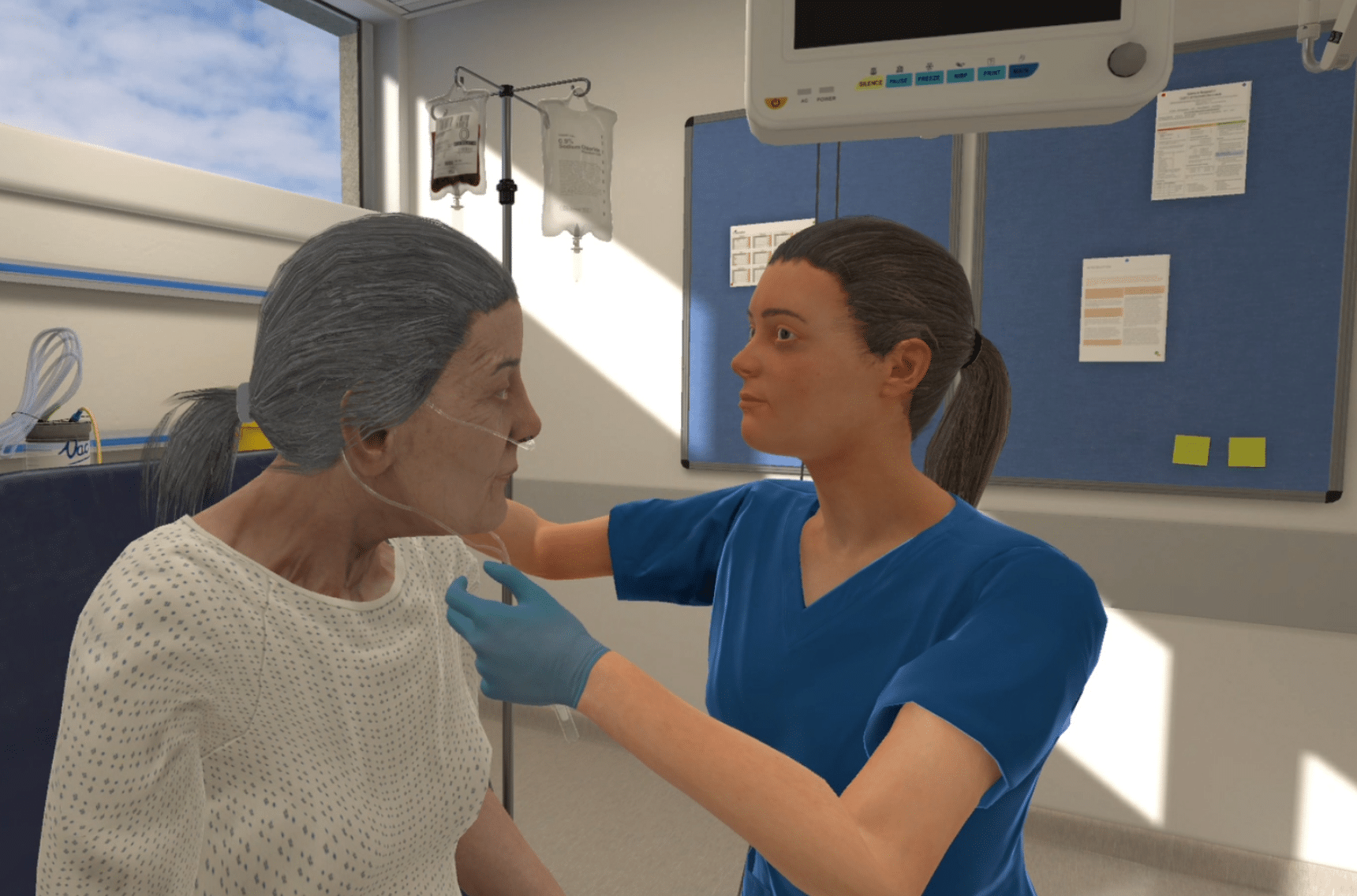
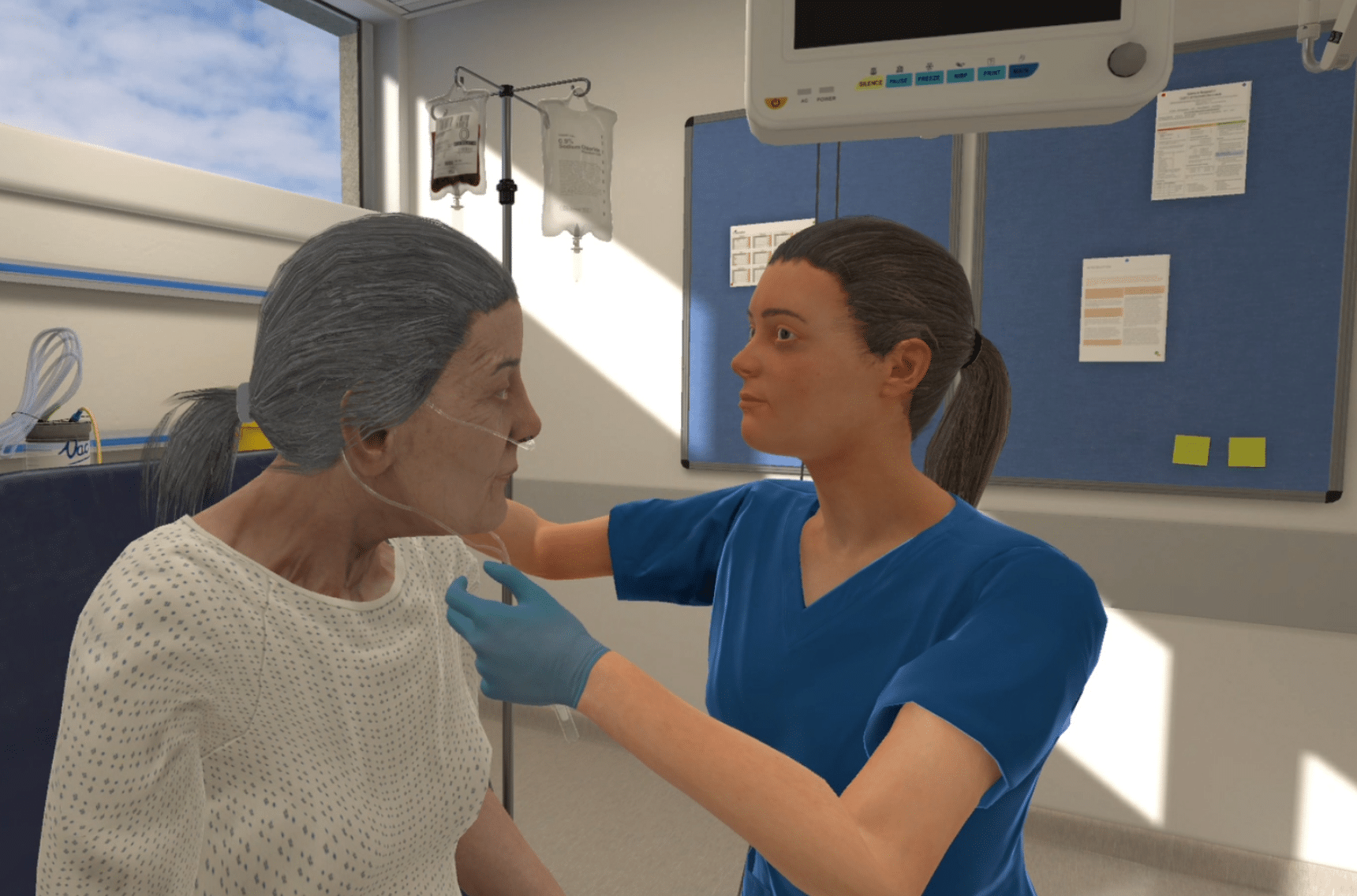
Voice Control
Develop and hone essential communication skills.
Speak directly with virtual AI-driven patients, caregivers, and colleagues to hone communication skills, build rapport, gather relevant information, and engage in difficult conversations.


Voice Control
Develop and hone essential communication skills
Speak directly with virtual patients, caregivers, and colleagues to hone communication skills - build rapport, gather relevant information, or engage in difficult conversations.
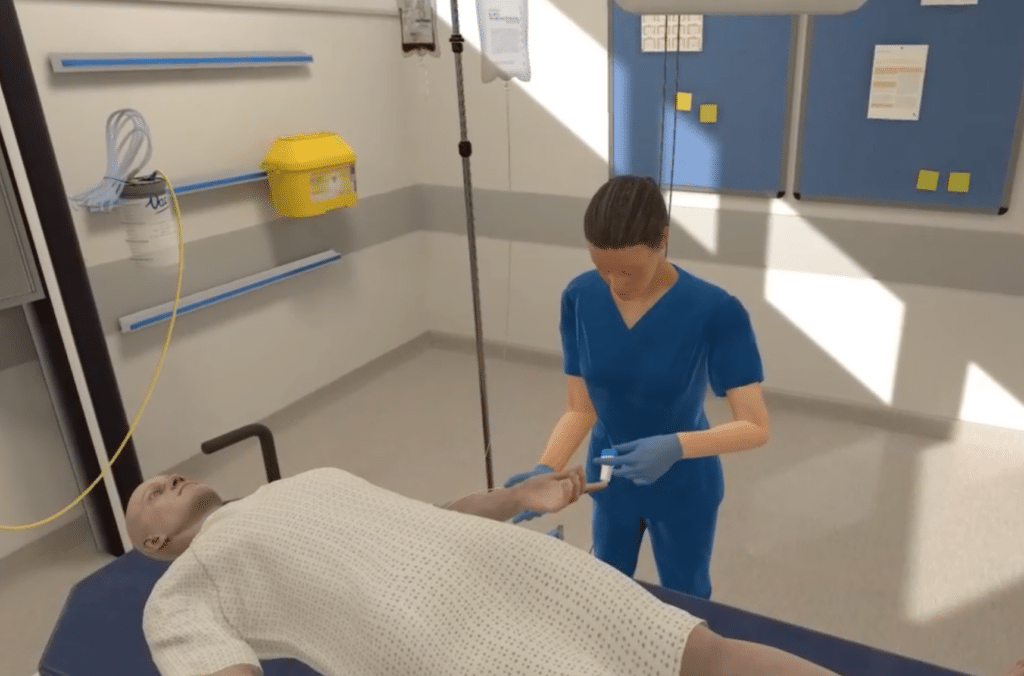
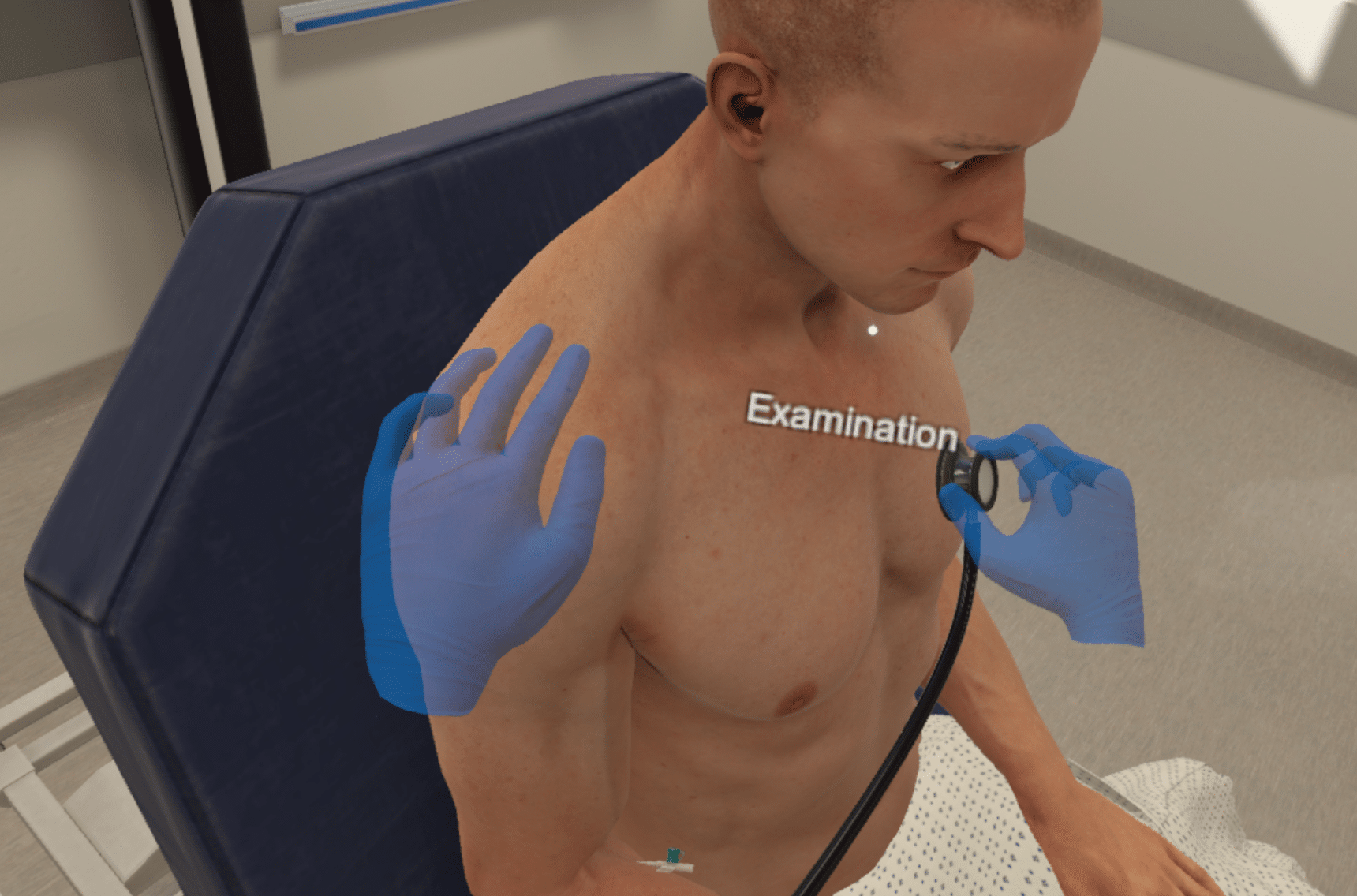
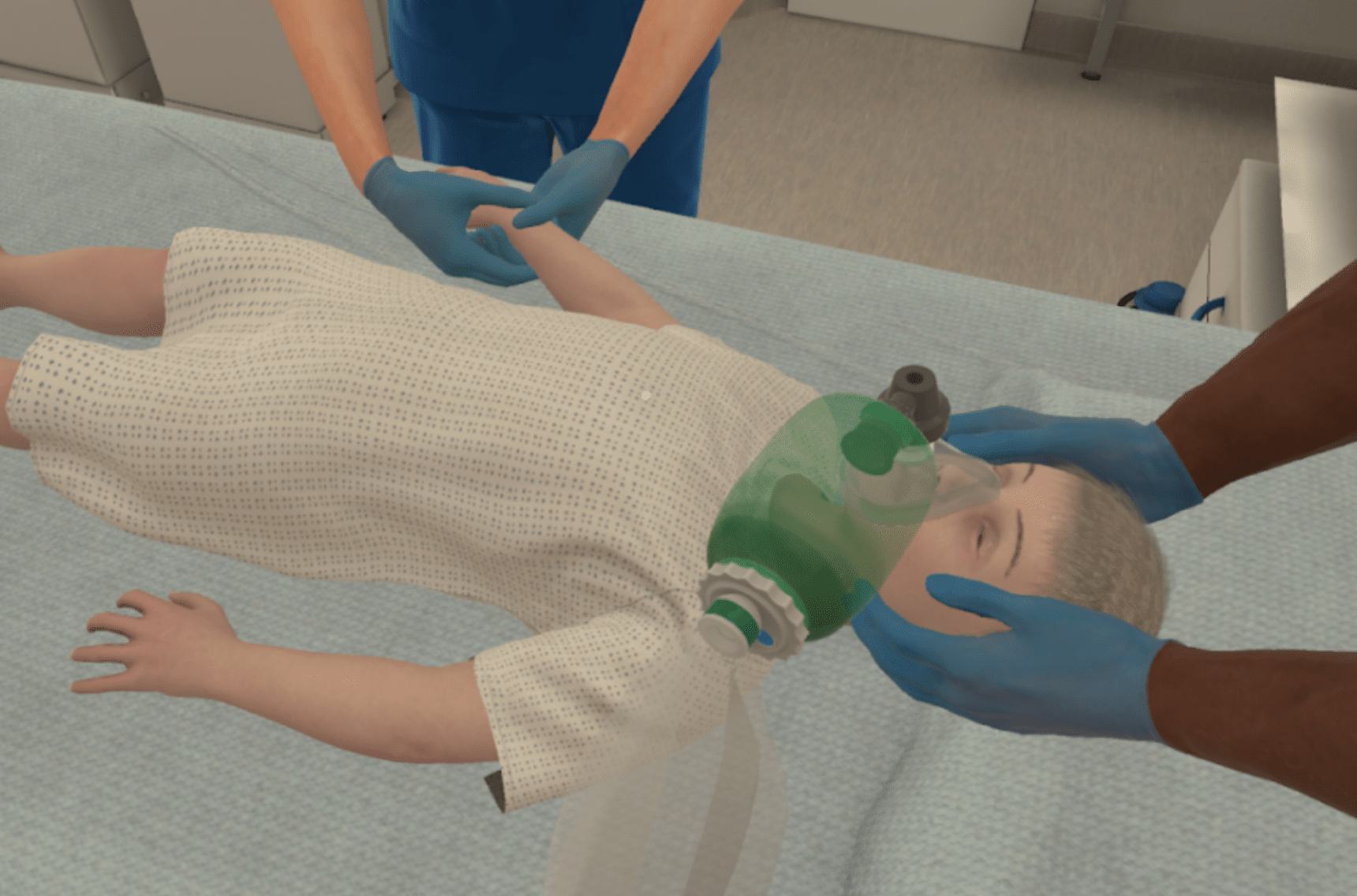
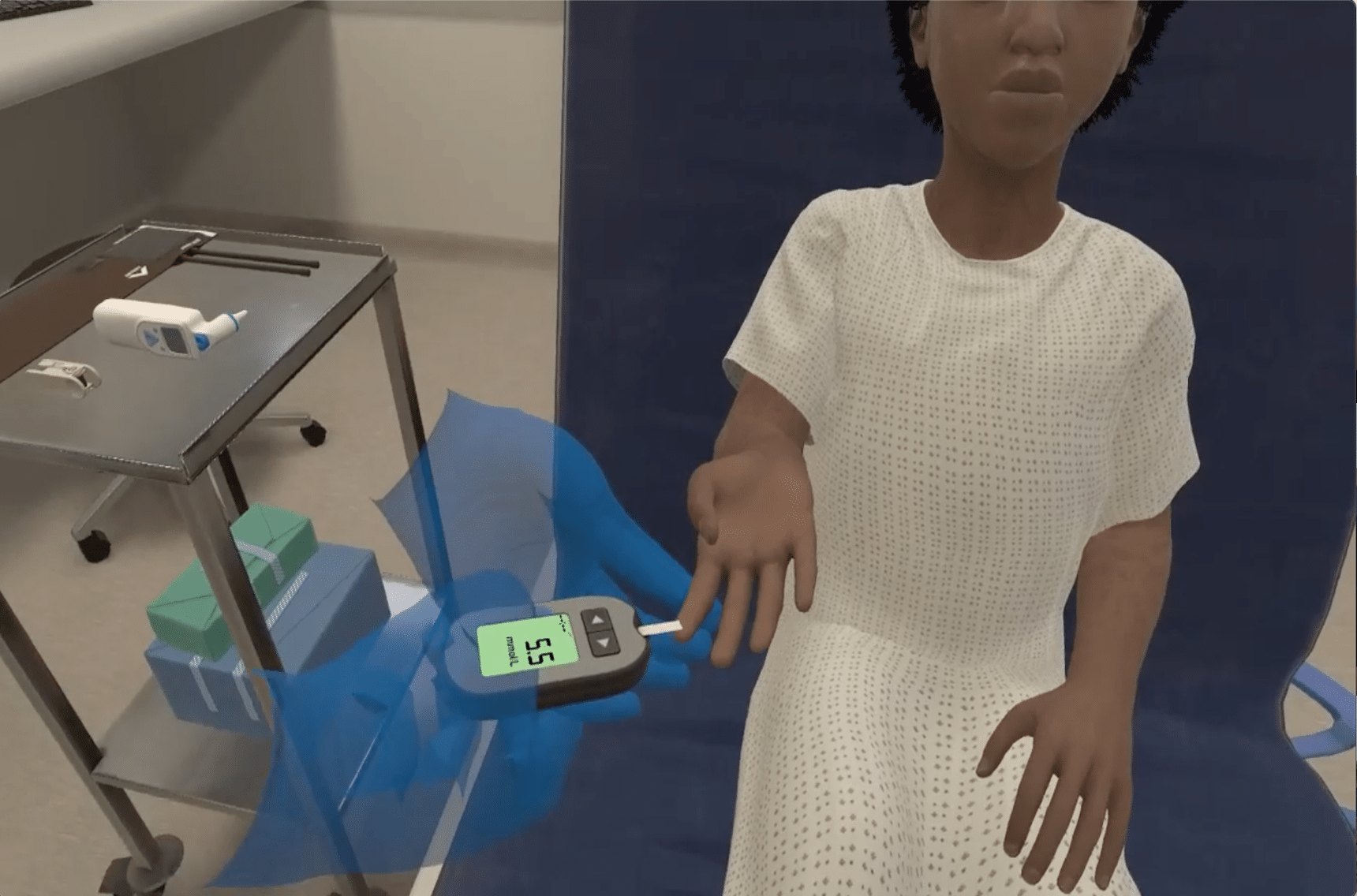
Hand Control
Develop psychomotor skills in procedural scenarios.
A step-by-step approach to develop core procedural skills in a clinical setting while engaging effectively with patients.
Sometimes, more is more.
More sim, more often with the OMS Scenario Library. From fundamentals & examination techniques to complex cases requiring layered skill sets, select from over 250 evidence-based scenarios to meet any learning objective.

Nursing Emergencies / MedSurg
Nursing Fundamentals

Nurse Practitioner
Pediatric Nursing
Clinic/Primary Care
Skills and Procedures
Physical Examination
Mental Health
Investigation/Interpretation

More scenarios coming soon

Nursing Emergencies / MedSurg
Nursing Fundamentals

Nurse Practitioner
Pediatric Nursing
Clinic/Primary Care
Medical emergencies
Pediatric emergencies
ACLS-ALS
Diabetes emergencies
Clinic/Primary Care

Physical exam

Investigation interpretation

Skills procedures
Interprofessional Emergencies
ACLS / ALS (Multiplayer)
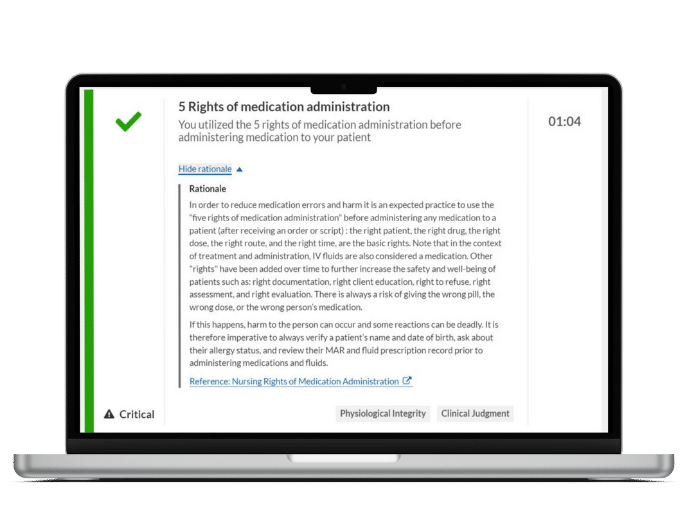
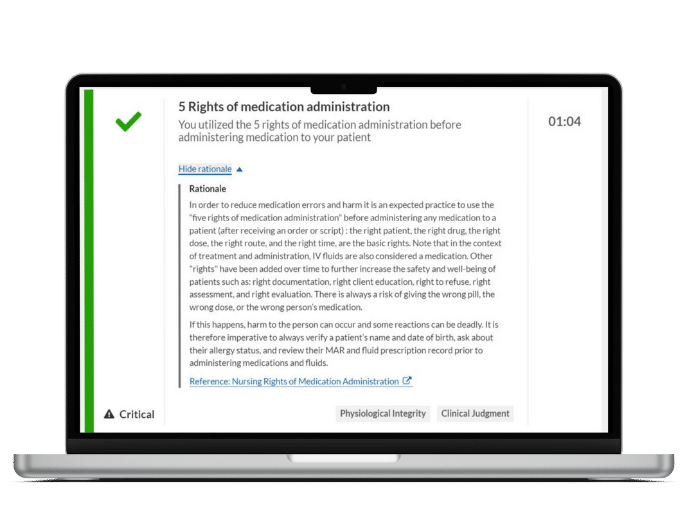
Immediate, personalized feedback
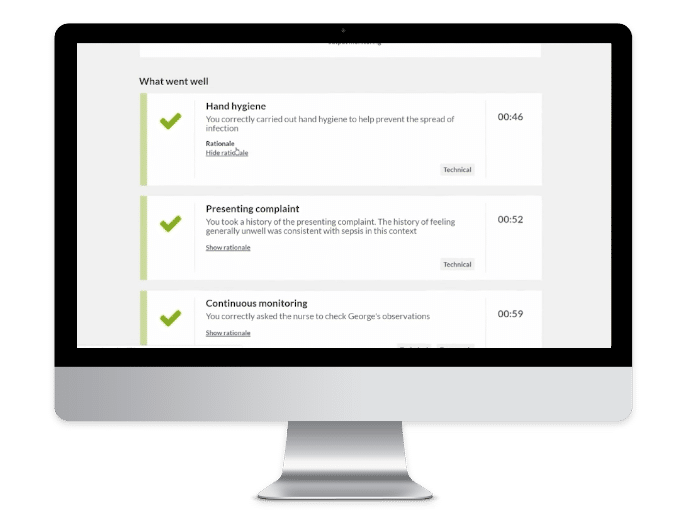
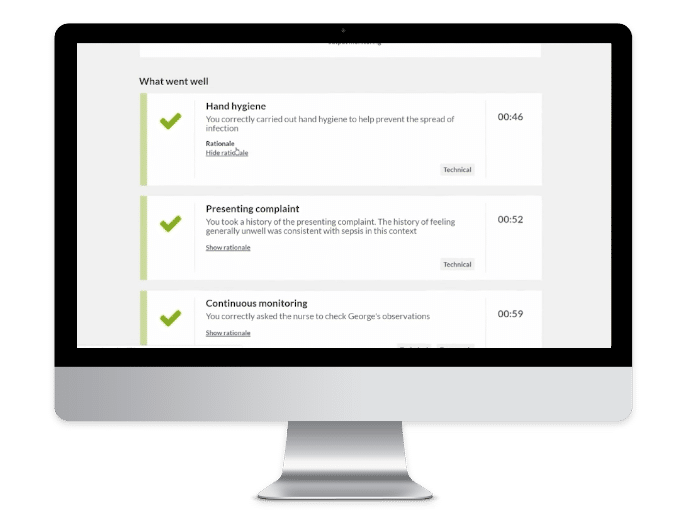
Immediate, personalized feedback

Precision data & analytics
Identify trends, remediate knowledge gaps, and gain insights on individual & cohort progress with a clinically-weighted scoring system and objective performance metrics to inform decision making.


Precision data & analytics
Identify trends, remediate knowledge gaps, and gain insights on individual & cohort progress with a clinically-weighted scoring system and objective performance metrics to inform decision making.

Competency Mapping & Tracking
Objectively track progress towards key competencies from 10 in-built frameworks, directly aligning actions in-scenario to core components of competency.
Competency Mapping & Tracking
Objectively track progress towards key competencies from 10 in-built frameworks, directly aligning actions in-scenario to core components of competency.
You can go your own way.
Tinker, tailor, or build out big changes to scenarios with OMS Create to meet your unique learning objectives.
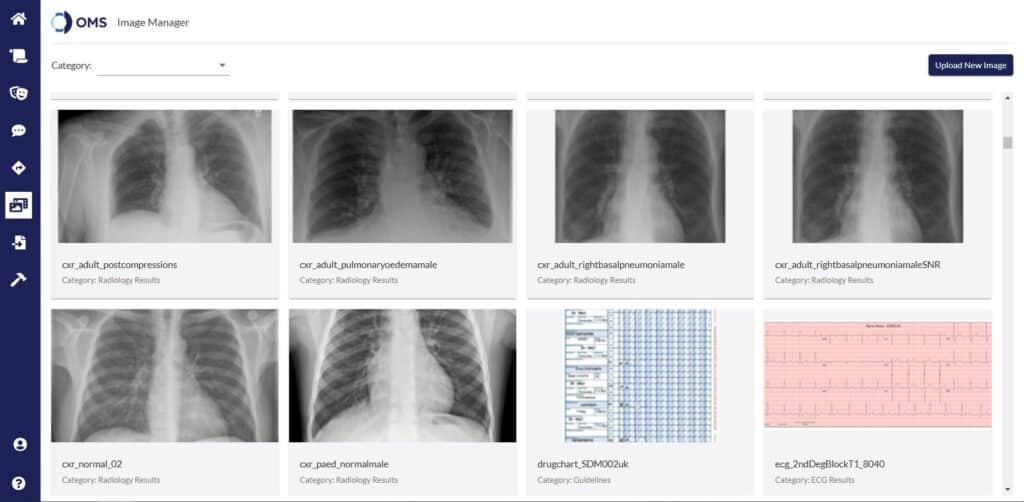
Make scenarios your own
Make adjustments to 250+ existing scenarios to meet your unique learning objectives. Align content with facility-specific protocol, change case complexity, or modify chart information for added specificity to any clinical situation.

Build your own blueprint
Craft clinical scenarios to align exactly with learning needs. No coding experience required – envision it, Create it.
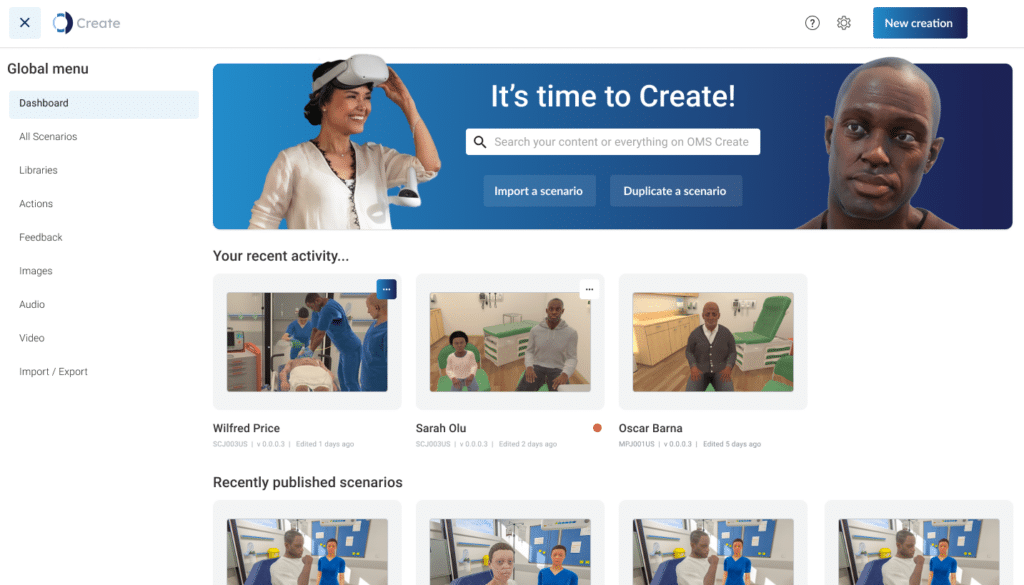
Be part of an industry-leading community
Participate in a community-driven information-sharing platform. Contribute to global initiatives and share ideas & scenarios with other VR pioneers.
OMS Create
The no-code authoring platform giving you the flexibility to customize existing scenarios or the freedom to be your own Clinical Author. Make any simulation bespoke to fit the needs of your organization.
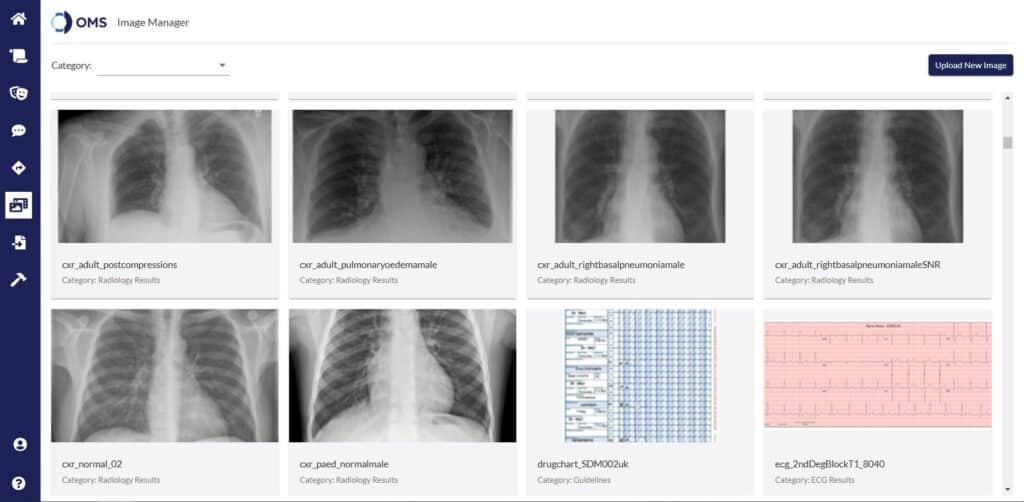
Make scenarios your own
Make adjustments to 240+ existing scenarios to meet your unique learning objectives. Align content with facility-specific protocol, change case complexity, or modify chart information for added specificity to any clinical situation.

Build your own blueprint
Craft clinical scenarios to align exactly with learning needs. No coding experience required – envision it, Create it.
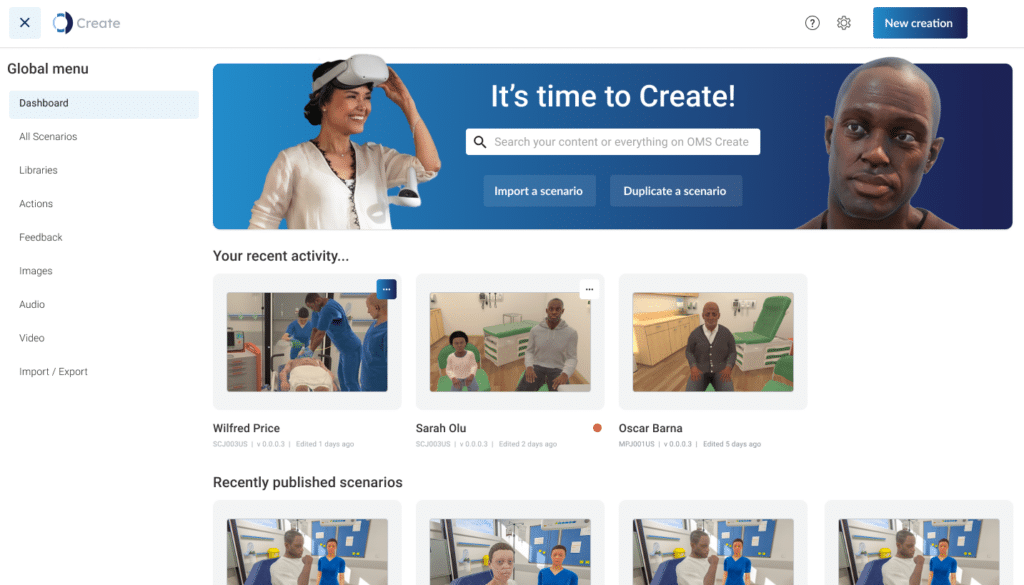
Be part of a leading-edge community
Participate in a community-driven information-sharing platform. Contribute to global initiatives and share ideas & scenarios with other VR pioneers.
Support at every stage.
We're better together...

01
Welcome
Customer Success Team welcomes you and stays in consistent contact as you start your OMS journey.

02
Onboarding
Coordinated, individualized onboarding sessions for technologists, admins, and learners.

03
Regular check-ins
Frequent touchpoints to monitor and assess progress in achieving your objectives.

04
Impact review
Feedback and review session at the 6 month mark to ensure you continue to see value from the OMS platform.