Preparing for the arrival of a new baby is often a time filled with joy, love, and anticipation as soon-to-be parents get ready both physically and mentally for a new chapter of life.
While pregnancy should be a time devoted solely to the excitement of bringing in new life, it sadly continues to be a cause for concern in healthcare with the CDC reporting a concerning rise in maternal death rate in the United States.
Rates of maternal mortality were dissected across a range of factors including age and race. For women aged 40 and older, the maternal mortality rate was 138.5 deaths per 100,000 live births, a rate 6.8 times higher when compared to a rate of 20.4 for women under 25 years old.
Significantly, racial disparities continue to be demonstrated in maternal mortality rates. According to the report entitled “Maternal Mortality Rates in the United States”, maternal mortality “rates for Black women were significantly higher than rates for White and Hispanic women.”
In a direct comparison, the maternal mortality rate in 2021 for White women was 26.6 deaths per 100,000 live births, while for Black women, the rate was at 69.9, 2.6 times higher than the rate for White women.
A recent study published by JAMA reviewed data between 1999-2019, While maternal mortality rates rose for all populations studied over 20 years, the median state maternal mortality rate was highest for Black women year over year.
In addition, disparities persisted in the median state maternal mortality rates for American Indian and Alaska Native women, as well, with rates more than tripling over the same time period.
While provisional data from the CDC demonstrates some promise in that maternal death rates appear to be decreasing, returning closer to rates seen pre-pandemic, this issue remains a significant part of maternal care.
Causes of maternal mortality
Taking in the above information, more questions surround why these disparities occur and what can be done to ameliorate them.
According to the World Health Organization, globally, major causes of maternal mortality can include infection, severe bleeding, or high blood pressure.
Infection or severe bleeding can occur following birth, however, cases with high blood pressure can impact or complicate delivery, making early detection and intervention highly important for patient safety.
Preparing for maternal healthcare
It’s well known that simulation-based education is a cornerstone of preparing for clinical situations that can arise at any time.
Between task trainers, manikins, or standardized patients, there’s a host of ways to practice delivering care in a safe space.
More recently, virtual simulation for maternal healthcare has become a pillar for healthcare education, providing another means to apply skills like clinical judgment and critical thinking to specific or infrequent situations related to specialized care.
Complications that arise during labor and delivery are difficult to recreate in physical simulation, often requiring specialized equipment and significant setup, reset, and takedown efforts.
Yet, it’s vitally important that learners – both students and practitioners – get repeated, frequent opportunities to grow accustomed to performing expertly in exactly these types of situations.
Particularly for onboarding nurses, recent graduates, or those coming from a generalist background – having the ability to lead in a high-intensity clinical situation before it plays out in real life can be invaluable to the preparation needed to feel competent, and confident, in delicate delivery situations.
Virtual reality and maternal care
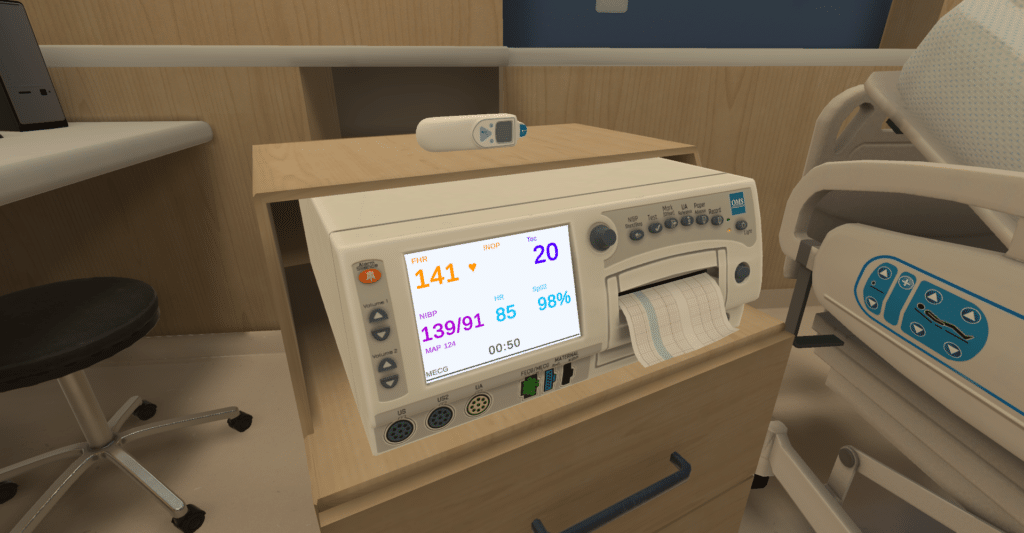
Virtual reality provides an immersive landscape to practice anything from fundamental and foundational clinical skills development to rare conditions and complex case management.
Within the OMS scenario library are over 240 existing scenarios, covering a wide range of nursing and medical foundations and specialties. The maternal health scenarios are created by our in-house team of Clinical Authors and undergo rigorous peer review to ensure alignment with current standards of best practice.

These scenarios were developed to address the need to remain prepared for the assessment and management of obstetric emergencies like preeclampsia.
An opportunity to apply clinical knowledge and decision making skills within the context of a case can help learners cement concepts and bridge the gap between theory and practice.
Learners take the lead – they alone decide on what tests to order, how to interpret results, and they are responsible for implementing an appropriate and timely treatment plan. They also get the opportunity to observe changes in patient condition and respond accordingly, an imperative skill set that remains difficult to replicate in physical simulation.
For more information
Particularly in maternal health, early detection and intervention is key in affecting positive outcomes and safe patient care. If you’re interested in learning more about this specialized content, get in touch with us to set up a time to talk. For more information on upcoming scenarios, sign up for our newsletter to keep tabs on what we’re up to and what’s coming.
