July 12, 2024
post
How to Bolster Critical Thinking in Nursing with Virtual Reality
In nursing, critical thinking is a vital and necessary skill. It’s not only critical thinking – clinical reasoning, clinical decision-making, and clinical judgment are all core components of nursing. While the nuances of these terms have been much discussed, they are all interrelated and function together as nurses observe, analyze, and take action. For example,…

In nursing, critical thinking is a vital and necessary skill. It’s not only critical thinking – clinical reasoning, clinical decision-making, and clinical judgment are all core components of nursing.
While the nuances of these terms have been much discussed, they are all interrelated and function together as nurses observe, analyze, and take action.
For example, nurses are often responsible for identifying cues of deterioration and escalating care quickly to prevent poor patient outcomes.
As novice nurses enter the field, there is significant concern about their readiness for practice, particularly regarding clinical decision-making.
One study reports that only about 20% of employers are “satisfied with decision-making abilities of new nurses”. Another study demonstrates that only about 9% of new graduate nurses meet the threshold for acceptable levels of competency.
There has been a push to address these issues with the Next Gen NCLEX, which is now measuring clinical judgment as part of the exam.
Considering that critical care nurses make a decision every 30 seconds, it’s clear how important it is to be prepared in all aspects of the clinical decision-making process.
Many institutions are now embracing technology like augmented or virtual reality to complement their didactic learning and their simulation programs.
Evidence supporting VR and critical thinking in nursing
Many of those core components of nursing practice, like clinical judgment, have several subcomponents.
Virtual reality and virtual simulation have shown positive impacts on factors like knowledge, critical thinking, and clinical decision-making.
In one systematic review, spanning 1996-2018, authors found that about 86% of studies showed positive outcomes on student learning with virtual simulation. That includes components like knowledge, skills, critical thinking, and – importantly – self-confidence.
The unique properties of virtual reality and virtual simulation allow for a new wave of practice that simply isn’t feasible in other forms of teaching and learning.
The flexibility of VR means that learners can access scenarios at any time, regardless of their location.
This means more simulation more often, and learners can repeat scenarios as often as needed to feel comfortable and confident in their clinical skills.
Learners can experience situations that would otherwise be impossible to recreate. Not only that, they can immerse themselves in these situations.
Even having one experience of a rare occurrence can be meaningful when the situation arises in the real world.
But how exactly do these simulations challenge and bolster confidence and critical thinking skills?

How to bolster clinical judgment using VR scenarios
With the OMS platform, learners can access simulations from a library of over 240 existing scenarios, across disciplines and specialties.
If you’re inclined, you can also align the simulations to competency frameworks.
Data collected during the simulation will be provided after the scenario is completed. Tagged actions and rationale will pinpoint the core components of your chosen framework with actions taken during the scenario.
For example:
Meet George ?

George is feeling generally unwell. While you’ll gain some information about his status from the nursing assistant, it’ll be up to you to figure out what’s going on with George.
Assuming you’ve performed your hand hygiene, you’ll want to introduce yourself to George, look through his chart, and gather information about what brought him in today.
As you learn more, you must filter out the most critical information to determine what to do next.
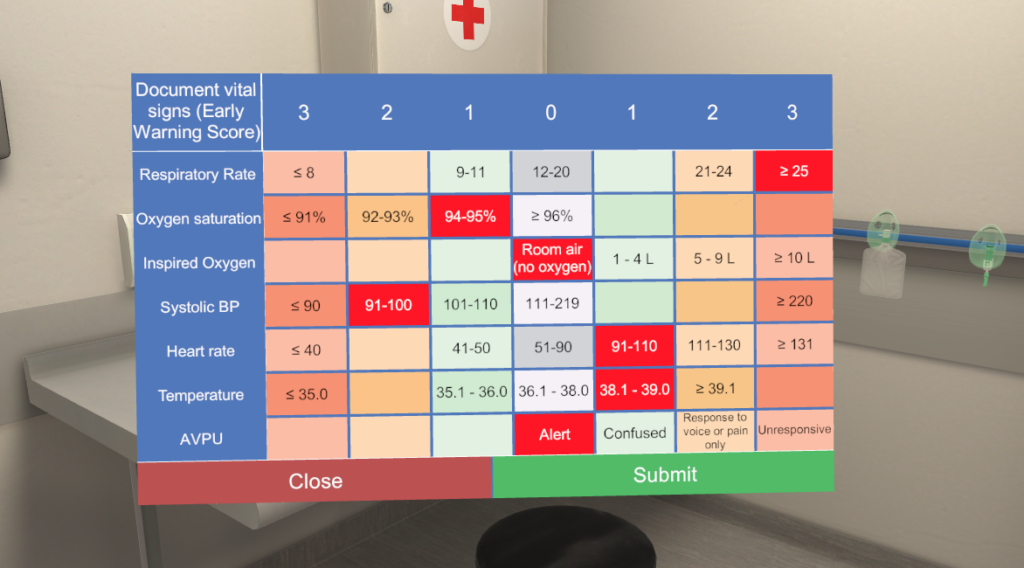
During your history taking, George mentions that he’s undergoing cancer treatment. As you assess his vitals, you note a high respiratory rate, low blood pressure, rapid heart rate, and low oxygen saturation. You also find that George has a fever.

Gathering the appropriate information and analyzing it speaks directly to the domains of clinical judgment – cue recognition and analysis.
At this stage, you’ll need to record your findings, use your information to start formulating a hypothesis, and decide what to do next.
If you’re suspicious of possible sepsis by now, you’d be correct in thinking that. George is acutely septic and will need urgent attention to prevent a worsening of his condition.
To arrive at this conclusion, you’ll need to have considered the relevant information and critically considered the patient’s case as a whole. His past medical history, current symptoms, and vital signs (alongside other tests and measures) all point to an acutely unwell patient. But it’s up to you as the lead to assess, prioritize, and formulate that hypothesis.
Because you’re concerned about the possibility of sepsis, you’ll need to determine the next steps to take in his care.
As the learner, you will need to do what you think is in the best interest of your patient. You will also need to determine when it’s appropriate to escalate care and provide an SBAR report to the wider team.
Then, you’ll need to take action to initiate treatment. With help from the wider team, you’ll have standing orders on medications to place, but it’s up to you to administer the medication appropriately and in a timely manner.
Once you’ve started treatment, you’ll also need to monitor and evaluate outcomes. Of course, you can decide to leave the room at any time, but only once you determine the patient is stable and safe.
If you’ve satisfied all of these components and determined the outcomes are positive, you’ve successfully utilized your clinical judgment to recognize and address an acute condition.
After completing the scenario, you’ll receive immediate feedback with rationale and tagged actions corresponding to your chosen competency framework.
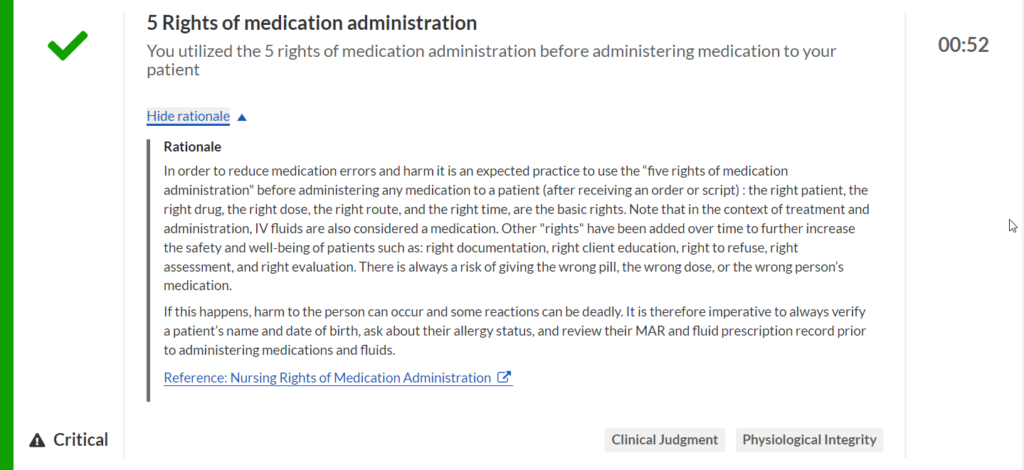
In the above image, you can see that you’ve successfully utilized the 5 rights of medication administration – which related to clinical judgment and psychosocial integrity.
If you’ve missed an action, like contacting the charge nurse, you can see why that action is critical, important, or additional. You can take that feedback as you continue your training and practice.
Having access to individualized feedback—with rationale, tagged actions, and links to resources—allows for deliberate practice and reflective thinking.
VR simulations like the above take you from start to finish in a safe learning environment. You can make mistakes and learn from them without fear of judgment or doing harm to a patient.
However, the immersive nature of VR scenarios means you’re the one in the room taking charge, and you’ll feel the empowerment of those decisions as you move through the scenario.
Leading a patient case from beginning to end is an opportunity that many students only have once they’re in practice, but with the opportunity to take the lead, learners can engage their critical thinking to make sound clinical decisions in real time, preparing them for real-world scenarios.
They can see the consequences of those actions play out. Because scenarios are accessible anytime, anywhere, learners can take feedback and immediately put it back into practice. Scenarios can be repeated as many times as needed for learners to build confidence, remediate knowledge gaps, and bolster their skills.
If you’re interested in taking a deeper dive into these scenarios, set up a time for a demonstration with one of our Educational Specialists.
Related
Ready to get real?
See how OMS can help your organization build confidence, competence, and clinical readiness for today’s healthcare.