January 3, 2025
post
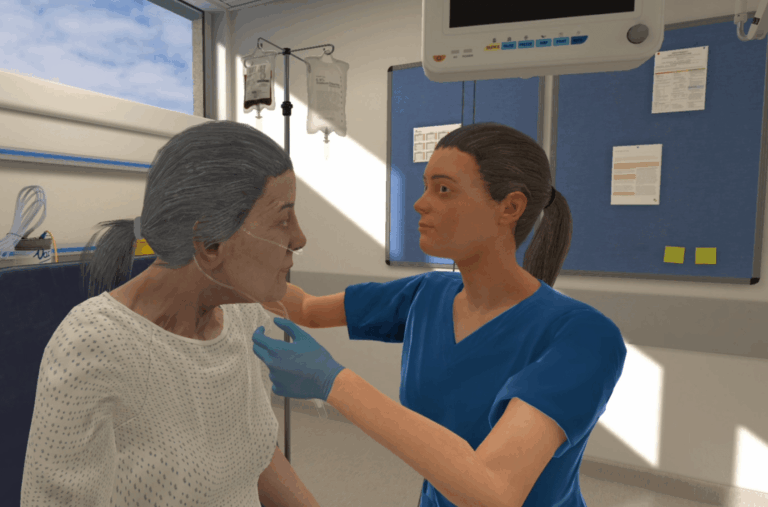
Virtual Reality or Manikin-based Simulation?
When it comes to healthcare training and education, simulation is a core component designed to apply, test, and refine clinical skills in a safe environment for the learner. There are many ways to accomplish this, from traditional methods like manikin-based simulations and the use of standardized patients to more modern methods like virtual simulation and…

When it comes to healthcare training and education, simulation is a core component designed to apply, test, and refine clinical skills in a safe environment for the learner.
There are many ways to accomplish this, from traditional methods like manikin-based simulations and the use of standardized patients to more modern methods like virtual simulation and virtual reality.
Which is better? Or perhaps a better question is, how do you decide which is the best fit?
We’ve taken a look across five different categories, comparing VR with traditional simulation methods:
- Cost & time
- Skill acquisition
- Realism
- Standardization
- Autonomy
Cost & time
Simulation, just like anything else, costs money and time to put together.
The amount of money can vary greatly, and much of that comes down to budget—what can or should a simulation lab spend to maintain or improve its simulation experiences?
Those decisions are made more individually, and depending on the equipment available and prior investments, what costs over the other can vary.
However, in studies directly comparing costs between virtual reality and manikin-based simulation, authors concluded that VR simulation requires 22% less time than physical simulation education and is 40% less expensive.
It’s no secret that manikin-based simulations take a long time to plan, set up, and run. In contrast, VR simulations can be run at the push of a button and may not require a facilitator. This can result in enormous time savings for faculty and educators.
Take it from the institutions that realize savings of 200 hours of time and reduce costs by 74%.
When it comes to cost and time savings, VR clearly has an advantage over manikin-based simulations.

Skill acquisition
It’s important that simulation do what you intend it to, which is typically to develop, hone, or refresh clinical skills.
Putting VR and traditional simulation head-to-head, there’s no clear winner. Both effectively develop clinical skills, and a cost-utility analysis found that VR delivers learning and performance outcomes similar to physical simulation while being significantly less expensive – a win-win!
Virtual reality is not here to replace physical simulation. All modalities of simulation have their own roles in connecting clinical concepts to application, and all should work together to support learners in their skills.
Boston Children’s Hospital is one such institution utilizing physical and VR simulation to help staff stay prepared for clinical situations.
Jeffrey Jacobs, XR Lead, Immersive Design Systems at Boston Children’s Hospital, said of VR simulation, “We expect VR simulation to take its place alongside physical simulation as a standard means for new people to train in and also experienced clinicians to learn new things.”
The choice is yours – it’s all about which modality is the best fit for educators and learners because both virtual reality and physical simulation are effective in the development of clinical skills.

Realism
Realism in simulation can be difficult to attain, but the more realistic the simulation, the better.
Both manikin training and VR simulation can be quite realistic. A high-fidelity manikin can do many things that a person would do and mimic many of the components of a particular condition.
Virtual reality can also be realistic, particularly in a headset, which brings another level of immersion to the simulation – something that can enhance the learning experience and bolster memory.
Many manikins or task trainers can only mimic parts of a larger whole, and when simulations are conducted in groups, it can inhibit the realism of the simulation.
In VR, the learner is individually transported to the virtual environment and works directly with a patient with a complete history and presenting symptoms. The narrative thread of a VR scenario creates a simulation where learners can get a complete picture of a patient’s status and see how their interventions impact those symptoms in real-time.
When it comes to realism, there is no clear winner – both VR and manikins can create a realistic environment for simulation. However, that largely depends on how the simulation is run, whether it’s done individually or in groups, the environment of the sim lab, and other factors that can either increase or decrease the realism of the scenario.
Whether you choose VR or manikin-based simulation, there’s more work to be done to ensure it’s as realistic an experience as possible.
Standardization
A concern for many healthcare students transitioning to practice is a limitation in clinical experiences. There can be a lot of fear around the realization that you may be caring for a patient with a condition you’ve only ever seen in a textbook.
It’s a common worry and informs the types of simulations that educators work to provide for students, but it’s nearly impossible to account for every condition a student may face.
Clinical experiences cannot be standardized – that is, not everyone will see the same conditions or get the same learning opportunities.
With a manikin-based simulation, often conducted in groups, it’s very difficult to recreate the exact same experience for every group of students over the course of the day.
The 9a group won’t often get the same experience as the 3p group. Even within groups, experiences may not be the same. Learner A may be quieter and more observant while Learner B may be more hands-on. This results in two different experiences, even in the same simulation.
Virtual reality is a stark contrast to that. Each learner gets into a headset individually and gets the exact same simulation as everyone else. Of course, the simulations themselves may play out differently depending on what each learner does, but that doesn’t take away from the fact that every learner in a headset will see the same patient, presenting the same way, with the same opportunity to apply their skills.
When it comes to standardizing simulation experiences, virtual reality is the clear winner of the day.

Breadth of content
If you wanted to pivot from an adult sepsis scenario to an obstetrics postpartum hemorrhage scenario, you would need to have a completely separate manikin for that change, and you’d need to set aside significant time to coordinate that change.
Because learners can’t be guaranteed experiences in the clinical setting, this means it’s up to educators to fill the gaps and provide learners with guaranteed experiences so they can be as prepared as possible for any situation.
Manikin-based simulation is limited when it comes to breadth, because certain manikins can do certain things, and an adult manikin is an adult manikin.
With VR, scenarios can cover just about anything – there are very few, if any, limits on what a virtual reality scenario can be.
Having access to a library of scenarios, like the OMS platform with 260+ scenarios, can make switching from one specialty to another seamless.
In the above example, if you wanted to have learners first complete a sepsis scenario and then move on to an obstetrics scenario, that would take maybe a few minutes in virtual reality. You’d simply need to exit one scenario, then select another, and you’re on your way.
Plus, there’s a lot of ways you can impact, change, or edit a VR scenario with access to an authoring platform, like OMS Create.
This gives you even more flexibility in the breadth of content you can provide, giving VR the edge over manikin-based simulation.
When it comes to virtual reality or manikin-based simulation, one is not here to replace the other. Both have value and contribute to the learning process, and while the modalities are different, the goal is the same – to help learners bolster their skills, get and stay prepared for any situation in clinical practice.
Ready to start your VR journey? Have a look at our guide in selecting a VR partner to help you jumpstart the process!
Conclusion
When it comes to virtual reality or manikin-based simulation, one is not here to replace the other. Both have value and contribute to the learning process, and while the modalities are different, the goal is the same – to help learners bolster their skills, get and stay prepared for any situation in clinical practice.
Ready to start your VR journey? Have a look at our guide in selecting a VR partner to help you jumpstart the process!
Related
Ready to get real?
See how OMS can help your organization build confidence, competence, and clinical readiness for today’s healthcare.