June 12, 2025
post
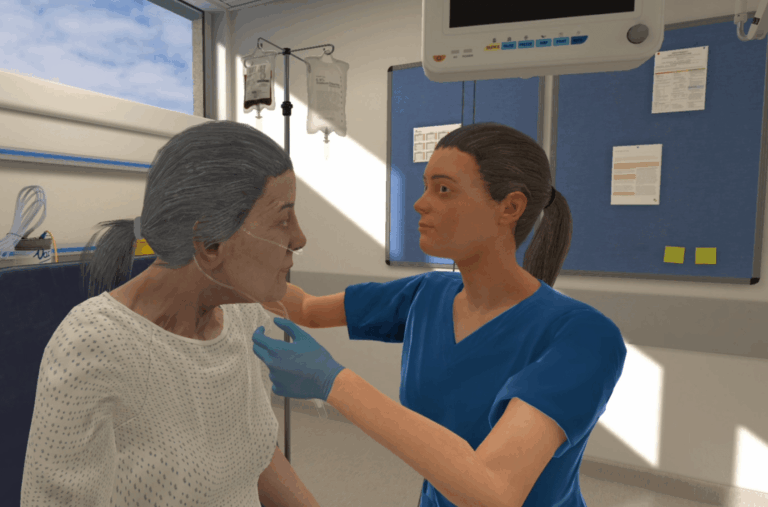
Reimagining Annual Competency Training with Virtual Reality
Each year, nurses are required to complete competency assessments or take part in programs that confirm their ongoing knowledge and skill development in patient care. Policies and standards, like those outlined by the Joint Commission, ANCC Magnet, or the Nursing & Midwifery Council, are meant to play a critical role in ensuring patient safety and…

Each year, nurses are required to complete competency assessments or take part in programs that confirm their ongoing knowledge and skill development in patient care.
Policies and standards, like those outlined by the Joint Commission, ANCC Magnet, or the Nursing & Midwifery Council, are meant to play a critical role in ensuring patient safety and practice readiness.
Amid growing complexity in healthcare environments and the expanding role of the practicing nurse, maintaining and developing clinical skills calls for both effective and engaging training methods.
Coordinating annual competencies can be challenging and often impractical. It’s especially difficult to bring nurses together at a specific time and place – particularly those working night shifts or other off-hours.
There’s a real need for effective and efficient training that realistically represents clinical practice – cut to, virtual reality.

Understanding Annual Competency Requirements
Competency training in the United Kingdom
Competency requirements vary – by state, region, or country.
In the United Kingdom, for example, the NHS has recently announced an updated Mandatory Learning Policy Framework that outlines requirements for annual competencies across various roles.
Some competencies are mandated nationally, others locally, while there are other competencies that are role-specific. In the NHS, for example, mandatory training includes topics like: sepsis recognition, anaphylaxis, infection prevention and control, and emergency response.
These competency requirements are designed to support inclusive, accessible, and outcome-driven education by encouraging a variety of learning methods, such as the use of a blended learning approach.
Competency training in the United States
In the United States, competency requirements for nurses vary by state, but ongoing clinical competency is typically managed by employers, not reported directly to the state board of nursing. State boards more commonly require continuing education or practice hours for license renewal.
Often, these competencies revolve around skills needed to provide optimal patient-centered care, like clinical or communication skills. If a nurse chooses to go down a more specialized path, that may change their competency requirements with additional, more specialized skills.
Safety, evidence-based practice, and interprofessional teamwork are often highlighted as core competencies, as well.
Demonstrating success in these competencies often requires training, and because nurses must meet these requirements to continue their practice, these sessions may or may not take place during work hours or on-site.
The use of a blended learning approach that pulls in both in-person and remote training can support the optimal and efficient training for these competencies.

The Case for VR in Competency Training
Virtual reality is just one piece of the puzzle, but it can be an effective and integral part of providing comprehensive competency training that’s immersive, engaging, and meaningful for learners.
In one study, 3 months after VR training, 89% of participants reported using what they learned in their everyday practice, and 96% agreed that VR scenarios were better for their knowledge retention than eLearning.
Carle BroMenn Medical Center, for example, has used virtual reality to support sepsis training, finding improvements in nursing confidence, competency, and to their facility metrics on overall sepsis management across the hospital.
Boston Children’s Hospital has also leveraged VR to enhance onboarding in the cardiac ICU, supporting general competencies and specific skills training for their nursing staff.
Virtual reality has several benefits that make it an ideal candidate for incorporating into competency training:
- Standardization: Certain VR platforms, like OMS, provide standardized clinical experiences, guaranteeing the same learning module for every learner, supporting reduced variability in care and expanding exposure to certain emergent conditions, like sepsis.
- Engagement: VR is immersive, and higher levels of immersion have been associated with improved memory.
- Scalability: With a VR platform like OMS, learners can access VR simulation both on site or at home (or anywhere else, for that matter!). This offers an accessible option for those who cannot tolerate a VR headset and provides a flexible option for completing training at a time that makes sense for each individual learner – any number of learners can access this training, making it a scalable option, as well.
- Data & analytics: Learners and educators can both access training data, providing individual or group-level insights. This can be used to quickly identify areas of remediation or opportunities for skill development.
For practicing nurses, getting to the right place at the right time for training sessions can be difficult, particularly if those sessions require a nurse to move off of the floor during a shift.
Often, the group size is limited or training may not be at an individual level.
Implementing virtual reality can provide greater flexibility and can reach learners at scale, wherever they’re located.
For more on using virtual reality to support competency training, get in touch with one of our Educational Specialists to talk through your institution’s specific needs.
Related
Ready to get real?
See how OMS can help your organization build confidence, competence, and clinical readiness for today’s healthcare.