OMS FOR ACADEMIA
Scale your sim program.
With or without faculty.
Give your faculty back their time. With OMS, you can both scale your simulation program and save 100's of hours of faculty time.
ON-DEMAND SIMULATIONS
The only platform that
can be run faculty-free.
With OMS, you can deploy training automatically, with or without faculty.
It allows you to scale your training efforts without compromising on quality, providing the flexibility your learners need to practice anytime, anywhere.

BETTER FACULTY-LED EDUCATION
Give your faculty real-life superpowers.
- Help them provide on-demand training for your learners with infinitely repeatable simulations.
- Help them provide consistent training, ensuring learning is objective and standardized.
- Help them provide a better learning experience with a variety of interaction modes.

UNLIMITED CLINICAL PLACEMENTS
Give every learner clinical experience.
After rolling out OMS, you can give your learners the clinical experiences they need to transition to practice easily.
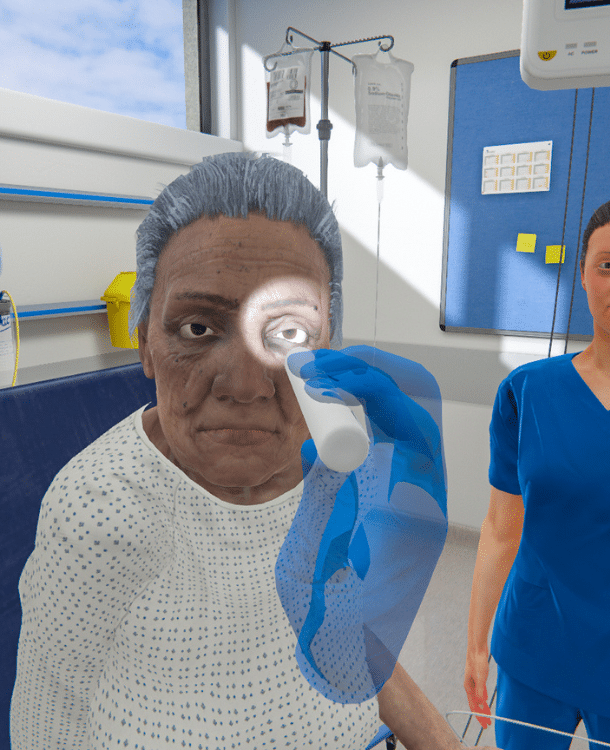
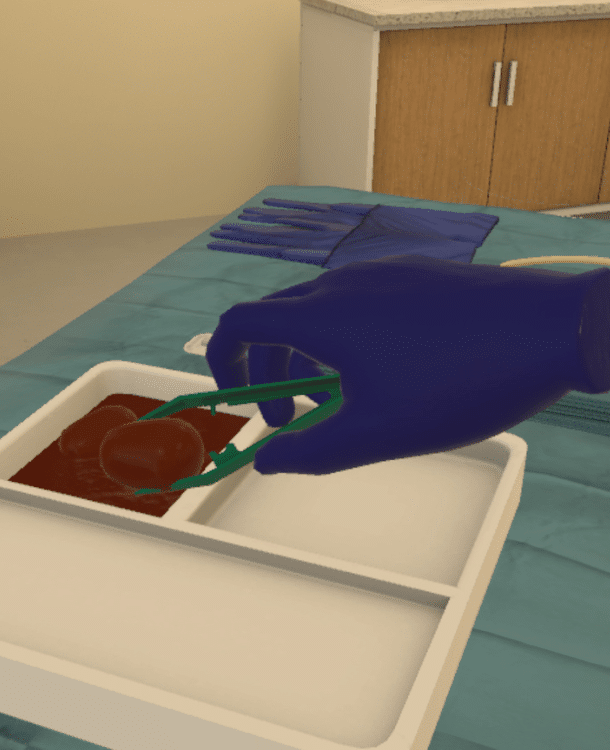
VR can simulate clinical environments, providing students with hands-on experience, in a controlled setting, and reducing the demand for physical clinical placements.
Save time. Reduce costs.
Improve training.

With or without faculty
OMS is a standalone system that can run without faculty intervention. Scenarios are infinitely repeatable, scaling simulation without increasing staff time.
Standardized & objective
Give every learner a chance to see specific clinical situations. Track progress and remediate knowledge gaps with objective data & analytics.
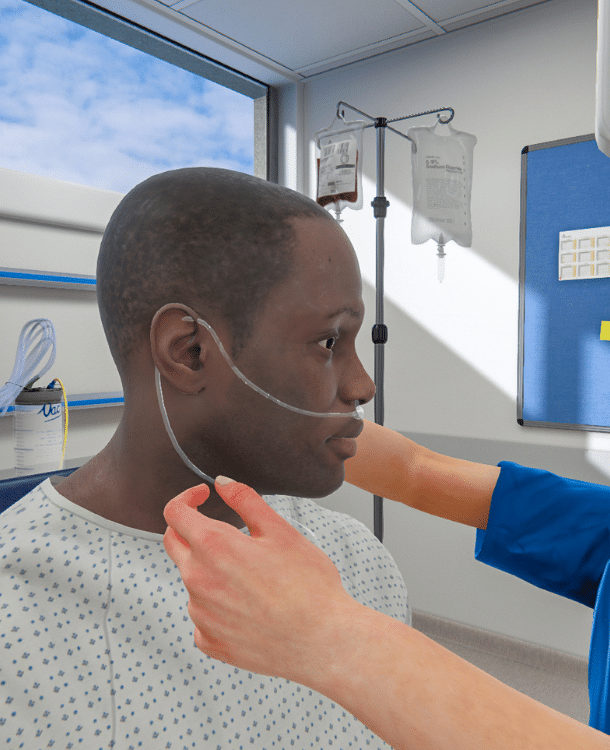
250+ diverse scenarios
With over 250 clinical scenarios across multiple specialties. They are designed to improve clinical performance, focusing on competence and capabilities.
VR or on-screen
OMS can run on-screen or in VR. Combining automation and availability allows institutions to run scenarios whenever and wherever they are needed.
Frequently Asked Questions
Find answers to questions Deans have on VR in academia!
Is VR expensive to integrate into our program?
While the price varies, adopting virtual reality in nursing can reduce time, equipment, and costs associated with simulation. One case study found that using OMS led to a 74% reduction in time and equipment costs compared to traditional simulation methods.
Other studies have shown similar findings, noting that VR simulation requires 22% less time and is 40% less expensive than physical simulation. A cost-utility analysis conducted by Haerling demonstrated the cost-utility ratio of virtual simulation to be $1.08 compared to physical simulation at $3.62 – the paper also found that while less expensive, VR ultimately delivered the same learning and performance outcomes as physical simulation.
Is VR here to replace physical simulation?
Not at all! Physical simulation is a cornerstone of nursing education, and it’s not going anywhere. VR is here to supplement didactic learning and support the development of clinical skills. VR is an accessible way for students to access experiential learning opportunities more often with fewer costs.
How steep is the learning curve when using VR?
Learning anything new can take some time to get your feet wet, and VR is no different in that way. For many students (and educators), VR has been reported as easy-to-use, highly-rated learning experience, and a tool 95.5% of learners would recommend to their peers.
To ease the transition, OMS recommends using prebriefing and orientation resources (which can be provided to you during the onboarding process) to support learners and educators in getting familiar with VR technology before ever entering a scenario.
Are VR nursing scenarios aligned with standards of best practice?
At OMS, scenarios are created by an in-house team of Clinical Authors who are clinicians, simulationists, and educators with a wealth of experience in healthcare education and direct patient care.
Clinical Authors use best practice guidelines to ensure alignment with standards of care, and all OMS scenarios undergo a rigorous peer review process to ensure a scenario is ready for release.
Are there different ways to interact in the simulation?
Yes! Depending on the learner level and objectives, different modalities allow for various levels of interaction in the simulation.
For example, a communication-based scenario allows the learner and the virtual patient to have a real conversation, leaving the simulation very open-ended for learners to build communication skills. Other scenarios allow for menu-based interaction or more hands-on interactivity for procedural skills.
What data do learners & educators receive from the simulation?
The OMS platform is a comprehensive learning tool that logs and tracks data for both learners and educators.
Learners will receive immediate feedback following a scenario with areas of strength and improvements alongside evidence-based rationale.
Educators are able to access individual or cohort-based data to identify trends and remediate knowledge gaps.
With the Competency Mapping & Tracking feature, data can be even more specific, bridging theory and practice by logging actions taken in scenarios and aligning them with the core components of a given competency framework.