September 26, 2023
Case STudy
How Carle BroMenn Is Using VR to Advance Sepsis Management
Overview As virtual reality continues to grow and become a mainstay of healthcare education and training, its uses are being continuously iterated and researched. Many academic institutions have rapidly adopted this technology and are using it to support students’ knowledge application, prepare them for clinical placements, or assess their skills. As those students graduate and…
Overview
As virtual reality continues to grow and become a mainstay of healthcare education and training, its uses are being continuously iterated and researched.
Many academic institutions have rapidly adopted this technology and are using it to support students’ knowledge application, prepare them for clinical placements, or assess their skills.
As those students graduate and head into practice, they may anticipate and increasingly expect healthcare systems to already use this technology as an adjunct to their training programs. In this way, VR can be a helpful addition to the recruitment process, using standardization to assist in decision-making and showing candidates the innovation and support they can expect at the outset. However, the uses of VR in health systems reach far beyond recruitment.
Carle BroMenn Medical Center spoke with OMS to discuss their implementation of VR to bolster staff education and positively impact patient outcomes (video above).
The Problem
Sepsis is a serious condition with cases that have been on the rise nationally for many reasons, per The National Institute of General Medical Sciences, which reports that approximately 1.7 million adults develop sepsis yearly and states it is a leading cause of death in hospitals.
The symptoms of sepsis, particularly in the early stages, can be seen in other, often more common conditions, making it difficult to identify quickly. Additionally, anyone can be affected by sepsis across a hospital system, making it an important piece of clinical knowledge for everyone caring for patients.
While many people who develop sepsis can have a full recovery, others may have lifelong consequences as a result. The intensity and complexity of treatment can place an increased financial impact on healthcare systems, making sepsis potentially costly for both patients and hospitals.
While life-threatening, signs of sepsis, when caught and treated early, can mean better potential outcomes for patients.
In order to support improvements in the recognition and management of sepsis across departments, the team at Carle BroMenn Medical Center decided to utilize virtual reality as an innovative way to provide education and training to their clinical staff on the early recognition and treatment of sepsis.
Angelia DeWeese, Simulation Education Specialist, said of the choice to target sepsis treatment:
“We are looking for improved patient outcomes. That’s why we’re doing this – the patient is at the center of it.”
We are looking for improved patient outcomes. That’s why we’re doing this – the patient is at the center of it.
Angelia DeWeese
Simulation Education Specialist
The Solution
Following their research on virtual reality for their use case, the team at Carle BroMenn Medical Center chose to work in partnership with Oxford Medical Simulation (OMS) to bring an immersive sepsis case to life for their staff.
The breadth and depth of the scenario library, the automated feedback, the robust and immediate data provided by the platform, and the collaborative and responsive nature of the OMS team were key features for the team at Carle in selecting their VR partner.
Once a determination had been made about the use case, the teams at Carle BroMenn and OMS worked together to develop the corresponding learning objectives and match the scenario exactly with the protocol of the hospital system, ensuring nurses were receiving standardized, comprehensive training specific to the facility.
The initial implementation of VR included sepsis training for nurses in both the Emergency Department and the Intensive Care Unit.
To start their use of OMS, nurses first participated in a pre-brief that included an orientation to the equipment, then completed VR training sessions. While the VR scenarios themselves take approximately 20 minutes to complete, training sessions lasted for up to two hours to accommodate orientation, the potential to repeat scenarios, facilitator feedback, and post-VR surveys.
The educators at Carle BroMenn decided on a benchmark pass rate for the scenario which they determined would fulfill both goals of demonstrating competency in the management of a sepsis case while providing room for learners to familiarize themselves with the VR modality to facilitate an overall positive experience.
Learners completed a questionnaire prior to and following the completion of their scenarios. Additionally, between scenarios, learners received immediate, automated feedback from the platform followed by a debrief with a facilitator, so that they were able to take the feedback and immediately implement it back into practice.
The initiative aimed to bring sepsis training to the forefront of nurses’ minds, with the goal to improve the time to recognition and early treatment of sepsis to positively impact patient outcomes.
The Rollout
The team at Carle BroMenn Medical Center looked at several metrics related to the sepsis case.
The OMS Score
The scoring system generated by the OMS platform is weighted based on clinical importance of the actions the learner takes, how they have prioritized these actions, and how they’ve worked as a team. For example, if a critical component of care is not completed efficiently or a safety flag is missed, it is not possible to receive a high score for that attempt.
In addition to the percent score provided by the OMS platform, evidence-based feedback is presented to the learner, as well. This feedback provides learners with insight into the actions they performed well and where there is room for improvement, alongside rationale for processes important to the case.
Data amalgamated by the platform gives information to both learners and facilitators about individual or group-based performance – educators at Carle BroMenn reported that OMS was easy to use, and they utilized the automated data provided by the platform to identify trends or gaps, and continue to adjust their education to close any gaps in knowledge.
From the first attempt to the last attempt, learners demonstrated an improvement in scores by approximately 22%, going from an average first score of nearly 61% to an average final score of just above 83%.
Self-perceived Confidence & Competence
Additionally, nurses reported an increase in their levels of confidence and competence in caring for a patient with sepsis.
Angela Turner, a Nursing Professional Development Specialist at Carle BroMenn, said of the impact that VR has had for learners:
“[VR] allowed [learners] to not only practice taking care of patients in a safe environment, but also allowed them to try a different modality, make mistakes within it, but know it’s safe and they’re not actually doing patient harm.”
On a 10-point scale, learners reported an average self-perceived level of confidence at 6.6 before engaging in VR simulations. After learners had the opportunity to conduct VR scenarios around sepsis, the average level of self-perceived confidence increased to 8.4.
With regard to self-perceived competence, learners reported an average score of 6.8 out of 10, pre-VR. Following the experience with VR simulation, learners later reported an average of 8.4 in their scores – nearly a 2-point increase in each category.
One participant, Sarah Huber, Quality Outcomes Coordinator Surgical Nursing, said of her confidence in managing sepsis after using OMS, “…Doing the VR did make me feel more confident in treating sepsis, and…the biggest reason is because of the feedback.”
Another learner, Kim Poling, RN2 on the Progressive Care Unit, noted that she took away a better understanding of roles of other nurses in different departments, stating, “As an inpatient nurse…there are steps that I don’t usually see that I think I would be more aware of because of the sepsis training.”
Overwhelmingly, learners enjoyed the VR experience and reported increased levels of self-perceived confidence and competence in caring for patients with sepsis, learning interventions they can implement as soon as they return to the floor.
Facility Metrics
As this work was focused on improving patient outcomes, the team at Carle BroMenn also looked at a set of real world measures that provided a percentage score for the management of sepsis across the hospital. The goal set was 75% for the facility.
During the months of February and March, performance scores averaged 49.5%. Following the use of VR within the Carle sepsis initiative, April and May showed scores of 88.7% and 89.0 % respectively.
As a Nursing Professional Development Specialist, Angela Turner, noted in conversation with learners following the use of OMS:
“Their scores moved, but it was bigger than that. Even in conversations with our learners after doing VR, as we were talking through, ‘What does sepsis really look like in real life?’…They could speak to, ‘These are all the things I would do’…and that’s what we were ultimately after – is that it translated.”
What’s next?
Learners were able to make mistakes in a safe environment that allowed them to effectively improve their processes and practices while engaging in the critical thinking needed to effectively manage emerging conditions like sepsis.
Just because nurses may work in the same hospital or facility does not mean they will have matching responsibilities, and with the completion of a holistic scenario around sepsis management, learners could walk away with a deeper understanding of the entire process of care, from start to finish.
With VR, learners are able to practice their skills in alignment with hospital policies and best practices in a safe environment, and have another learning experience to ultimately impact patient care.
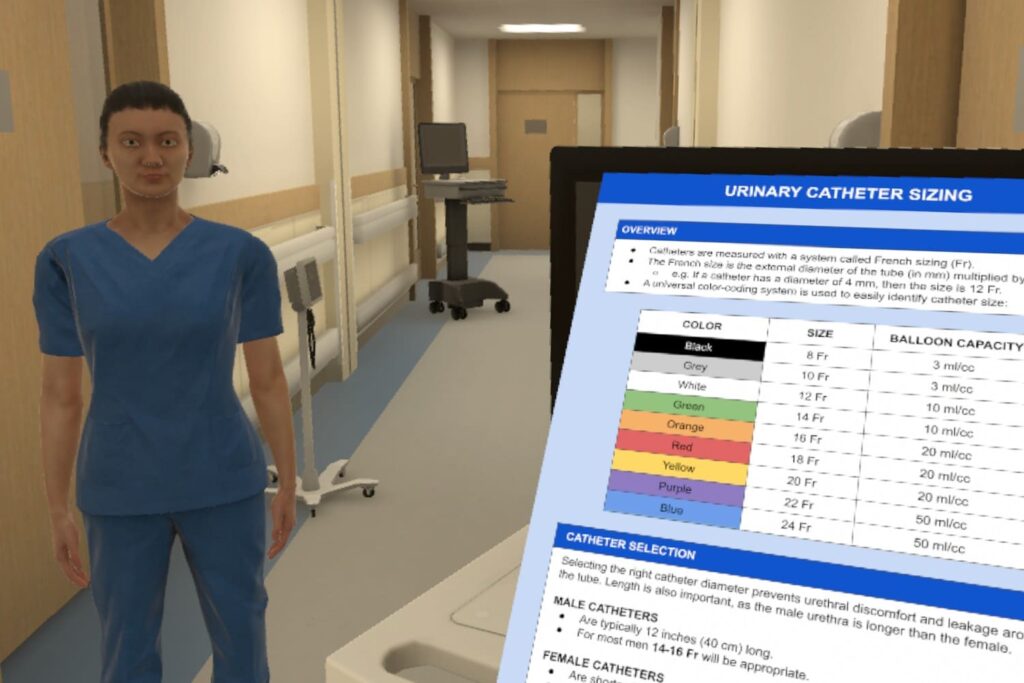
With such positive results, the team at Carle BroMenn has already expanded the use of OMS for other initiatives, including catheterization training with the urology clinic, and the team has plans to continue VR sepsis training with Carle Foundation, at a system-wide level.
As Simulation Education Specialist, Angelia DeWeese, notes:
“This was also a system initiative for Carle Health, so I am excited that we have done this at a facility level, but also it’s opened up the door for our system to be looking at this too. For that opportunity to impact…outcomes from a system perspective is exciting.”
Additionally, Carle BroMenn Medical Center is excited to expand their use of VR with additional scenarios that they may use with new graduates, including other clinical topics to bolster continued education of new healthcare professionals.
VR allowed learners to not only practice taking care of patients in a safe environment, but also allowed them to try a different modality, make mistakes within it, but know it’s safe and they’re not actually doing patient harm.
Related
Ready to get real?
See how OMS can help your organization build confidence, competence, and clinical readiness for today’s healthcare.

