June 1, 2021
post
How We’re Challenging Unconscious Bias to Progress Healthcare for Transgender Patients
It’s time to open up a dialogue with healthcare professionals around gender identity and mental health.

It’s time to open up a dialogue with healthcare professionals around gender identity and mental health.
Though we are becoming acutely aware of the importance of mental health, transgender patients continue to suffer significant barriers to appropriate care, including discrimination and a “lack of cultural competence”. This is especially concerning given the prevalence of mental illness amongst transgender individuals – recent research has found that the community are six times more likely than the general population to have a mood or anxiety disorder. How can we improve the care we provide transgender patients?
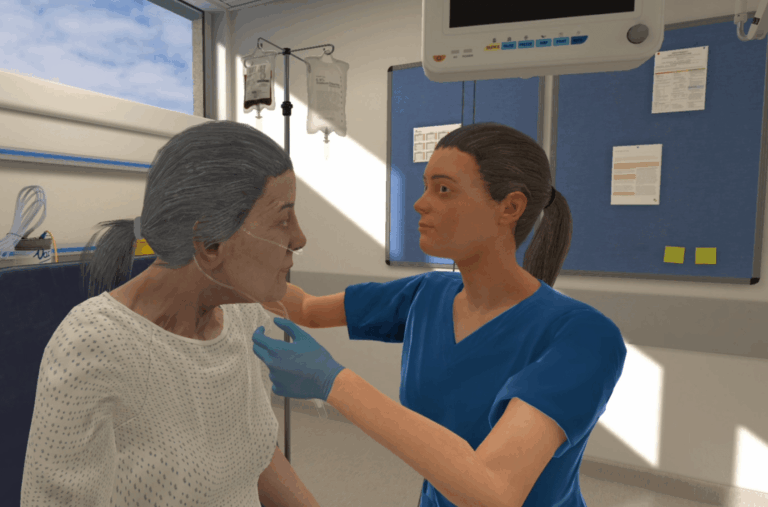
At OMS, we’ve created a new mental health scenario to challenge clinicians’ unconscious biases. Here, users encounter an adolescent patient, with the birth name Oscar, who has been admitted to hospital after a suicide attempt. Through a supportive and understanding dialogue, we learn that she is gender transitioning and prefers to go by the name of Ola.
We spoke to Dana Plank, RN – a nurse in New Hampshire – and Dr Bex Thompson – a physician in the UK – to get a better understanding of its significance. Both are clinical authors at OMS and have been instrumental in the scenario’s development.
We know how important mental health is, and how impactful these scenarios can be. In fact, mental healthcare and health inequalities are areas OMS actively works to improve. But this one resonates with so many people – we’d love to hear how it got started.
Bex: One of our authoring team (Kelly) had a great background in mental healthcare and was very passionate about making scenarios that aren’t just out of a textbook, but really bringing them to life and making them a bit more real-world. Kelly had worked with transgender people before and had first-hand knowledge and recognized how important the topic was. It’s one that’s not talked about enough in healthcare, and we saw an opportunity to change that.
What had been your experience of training on transgender awareness before working on this scenario?
Bex: Certainly when I went through med school (UK) we didn’t receive any formal training about how to approach topics around gender identity.
Dana: It’s the same here (US). LGBTQ issues aren’t something that we’re very good at—we’re not very good at using the right terminology and consistently demonstrating compassion towards these issues. But it’s just because we haven’t had the practice. The idea behind this scenario was to give people the opportunity to learn how to interact compassionately, and to ask the right questions so that you don’t alienate your patient.
You received input from people with first-hand experience of transgender issues to help develop the scenario. How did their expertise influence the finished product?
Dana: We mainly asked for our subject matter expert’s input to ensure we were representing the patient sensitively, and to find out whether we’d overlooked any issues they’d faced in the patient’s care. They have experience with transgender patients and mental health care as an RN, but they also identify as non-binary, which meant that they were able to offer both professional and personal insight. They certainly helped us with some background that we would’ve never thought of. For example, how the parents refer to this gender transitioning adolescent. If you’re calling the parents, it gives you an idea of how they feel. They might either be accepting of the situation that the patient is going through, or they might still refer to them as Oscar.
Bex: I also consulted with a colleague of mine who is training to be a psychiatrist. She helped us to narrow down the scenario and remove any unnecessary elements that could distract users from focusing on the patient’s mental health.
You mentioned taking out unnecessary elements. Can you tell us more about how the scenario developed to focus on the patient’s mental health?
Dana: Originally the patient had ligature marks – they weren’t gruesome, just a minor abrasion or burn. But Bex mentioned that from a doctor’s perspective, any kind of mark like that would suggest a more serious suicide attempt, needing a more serious physical examination. We didn’t want to go down that path – we wanted it to be mental health-focused – and our authoring approach got us there.
Bex: The patient was also originally drinking and using drugs, but we had to pare it back or it would’ve ended up being a child safety issue. It’s difficult because in real life, people do present with lots of things, but we have to be mindful that this is only a 20-minute scenario. At the end of the day, it’s a mental health scenario, so all the objectives are about understanding your patient and what led them to feel the way they do.
Even after it was stripped back, the scenario still sounds uniquely complex – a juvenile patient who is transitioning and has also attempted suicide. Was that a conscious choice?
Dana: This particular scenario is in an ED setting, so we needed something that would bring a patient there. It might look like a physical problem but in reality, it’s a mental health issue.
Bex: Absolutely. Our first few mental health scenarios were more simplistic, like an anxiety attack. It was a conscious decision, we were focusing on learning outcomes. But people don’t tend to come with just one problem. People are complicated, and this scenario reflects that. A gender transitioning patient is new for our scenarios but we should ideally be asking everyone their preferred pronouns and treating everyone with that consideration.
Why do you think that patient-focused care is so crucial for mental health scenarios like this one?
Bex: With anything you do in medicine, it should be about patient care and compassion, but with mental health in particular it’s so important. If you’re treating somebody’s heart attack and you don’t get on well, they might not like you, but you can still treat the problem quite successfully. That’s not the case with mental health – if you don’t connect with your patient, you’re really going to struggle.
How would you respond to those who would say mental health should only be treated by those within the specialty?
Bex: I think that’s wrong. As we have said, mental health often goes with physical problems and we have to take that holistic approach. Some problems you do need to separate, so you wouldn’t want a surgeon looking at a cardiology problem, but mental health filters into every part of medicine. It’s really important to understand mental health presentations because if someone’s having an anxiety attack and they’re short of breathing and having palpitations, I need to take a good history to make sure they’re not actually having a heart attack. They’re not just ‘patients’, we want to treat them as people.
Dana: We talk about “holism” in treating a patient. People are multifaceted beings, and everything that is affecting them physically, mentally, socially – everything comes into play. This holistic approach is emphasized in nurse training. You would be doing a disservice to a patient to not consider a whole person.
Bex: And even though this scenario is set in the ED, it could just as easily be used for other situations, such as for someone who is on a ward or even the community. The mental health scenarios help users to take the patient’s history and to recognize what’s going on, and that’s an important part of a clinician’s work. Whether you’re on a ward or in an outpatient community, you’re going to come across mental health.
Finally, why do you feel that this scenario is so important to furthering the understanding of transgender patients’ struggles?
Dana: I had an experience a little while back where I was describing this scenario to someone I knew, and saying that we can be better equipped by using the right pronouns, things like that. And he said, “What, just so they can be special?”. But you have to think about it from their perspective. Transgender individuals have been marginalized and treated unfairly their whole life. It’s not giving them special treatment – it’s giving them the same respect that we give everyone else. We are up against that lack of understanding and that’s why this scenario is so important.
Bex: Even if you understand why we need to be aware, a lot of people are uncomfortable because they haven’t come across the situation before. You might never come across it again. There are so many things going on for a clinician and it can be hard to remember things like asking patients’ pronouns, which is why normalizing it in this way is so important. It might feel a bit uncomfortable at first but that’s okay, you’re trying, and that’s key.
Dana: Absolutely. The fact that you’re acknowledging it and trying your best for the patient really speaks volumes.
About the Clinical Authors
Dana Plank MS, RN, CHSE
Dana is a Registered Nurse with a Masters in Nursing Education. Dana is also a Certified Healthcare Simulation Educator. Gaining extensive experience in OR Nursing, homecare, and public health, Dana then transitioned her career to simulation education. Since 2019, she’s been using her expertise to develop immersive sim scenarios as a Clinical Author at OMS.
Dr. Rebecca (Bex) Thompson BSc, MBBS
Bex is a Physician and Simulation Educator with a PGCert in Clinical Education. While working as a hospital physician she began delivering innovative simulation training, and developed specialist knowledge of clinical teaching. Bex continues to practice clinically alongside her work at OMS, and uses this real-world experience to help create engaging scenarios for learners as a specialist clinical author.
Related
Ready to get real?
See how OMS can help your organization build confidence, competence, and clinical readiness for today’s healthcare.