You’ve done the prep work, completed the simulation, and now it’s time for your debrief – one of the most critical components of the entire simulation experience.
Why is that?
Given that a significant amount of learning takes place at this stage, it’s important to take full advantage of the debrief session. It’s equally important, if you’re the facilitator, to set it up for a successful session with your learners.
What is debriefing?
The Healthcare Simulation Dictionary broadly defines the debrief as “a formal, collaborative, reflective process within the simulation learning activity”.
Often, educators and learners come together to analyze what happened in the scenario, discuss key concepts and takeaways, and ultimately encourage reflective thinking in learners, so that they can remediate gaps in knowledge and improve future performance.
It’s a time for learners to freely think in a safe learning environment and delve more deeply into their rationale, how they approached the case, and what they could have done differently to optimize the outcome.
Essential components of a debriefing session
While there are many debriefing approaches to choose from, such as instructor-led versus self-guided, or in-person versus virtual, there are several commonalities between the various methods that make for an intentional and successful debriefing session.
The Healthcare Simulation Standards of Best Practice (TM) has a section dedicated specifically to the debriefing process – which they say can include feedback, a full debrief, or a guided reflection.
Of course, aligning your session with evidence-based concepts is a must and is a good place to start. For example, it should be planned, structured, and related to the context of the simulation that just took place.
Because this can be a time to acknowledge and analyze mistakes, it’s critical to maintain psychological safety of the learners throughout the process, meaning learners should receive unbiased feedback from a credible source who remains non-judgmental and encourages self-reflection.
Remember that the goal of a debriefing is to facilitate reflective, critical thinking by the learner, so that they are able to apply that type of thinking to their everyday practice.
It’s also a tool to identify and address gaps in knowledge and ensure the transfer of clinical skills is progressing.
How do different methods of debriefing stack up?
You may already be familiar with the 3D debriefing model, which breaks down the process into three phases – defusing, discovery, and deepening – or perhaps you know the PEARLS method well, also referred to as Promoting Excellence and Reflective Thinking in Simulation.
There are many different debriefing techniques you can choose from, and it’s ultimately up to you to decide which one best supports your learners.
Beyond the framework you decide to employ, you’ll also need to decide whether to have your debrief be in person, virtual, or self-guided.
One study took a look at in-person, virtual, and self-guided debriefing methods following a virtual simulation and compared them against self-efficacy, knowledge, and overall experience scores.
All groups made improvements to their self-efficacy and knowledge scores, with no significant differences found between those who debriefed in-person versus virtual versus self-directed.
However, when it came down to the experience scores, the self-directed group differed from the other two group on the following items:
- Opportunity to resolve unsettled feelings
- Have questions answered about the simulation itself
- Have appropriate guidance
While the self-directed group were less satisfied in the above areas, they actually performed at similar standards compared to the other two debriefing groups.
These findings are consistent with other studies that have found improvements in performance outcomes across varying debriefing methods. However, it remains that faculty and staff must consider the advantages and disadvantages of each method and the needs of their learners to determine the type of debriefing that will serve their learners best.
The good news is, there are options!
How a virtual debrief differs from in-person
As the world continues to acclimate to a hybrid of in-person and virtual environments, it’s important to consider the use of both in-person and virtual facilitated debriefing sessions with your learners.
It is important to note that there are inherent differences between these types of sessions, which may influence how you conduct your debrief.
Remember that psychological safety is absolutely paramount in a successful debriefing. Creating and maintaining it requires three key components:
- The ability to make mistakes without fear of repercussions
- The qualities and credibility of the facilitator
- The use of foundational activities to prepare and orient participants
In many instances, this begins with a thorough prebrief, providing learners with clarity upfront. A prebrief sets the stage for psychological safety in simulation, particularly when it includes other components like demonstrating respect and care for learners and establishing the logistics of the simulation ahead of time.
In essence, prepare your participants with an orientation of the platform, whether in-person or virtual. Provide clear expectations and learning objectives, so they can be fully prepared for the simulation itself and the following discussion.
The need to maintain psychological safety is true wherever you are, but in the virtual world, there can be a few other recommendations that might help your learners feel more comfortable.
One group of nursing educators compiled a list of their experiences and recommendations for conducting virtual debriefing sessions.
These include:
- Allow flexible scheduling for students
- 6-10 students per group to encourage participation
- Cameras can be on or off
- Clear expectations about:
- The debrief session
- The recording of sessions
- Whether learners will be evaluated
- Regularly check the chat box for comments and questions
Although it may look a bit different from in-person discussions, virtual debriefing can be successful in helping learners process and analyze their experiences in simulation.
How can OMS bolster debriefing sessions?
The evidence is clear – there are many ways to conduct your debriefing sessions using best practices, and it’s very important to make these sessions a priority to encourage learning and the transfer of knowledge to practice.
Encouraging learners to think critically about their approach is essential, and tying key concepts and takeaways into learning objectives is meant to promote reflective thinking that learners can take with them anywhere.
For example, if one of your learning objectives involves prioritization of care, you may ask your learners to provide rationale for why they decided to continue working with one patient versus going to see another in a multi-patient scenario, or they may be prompted to think about their approach soon after they complete their simulation.
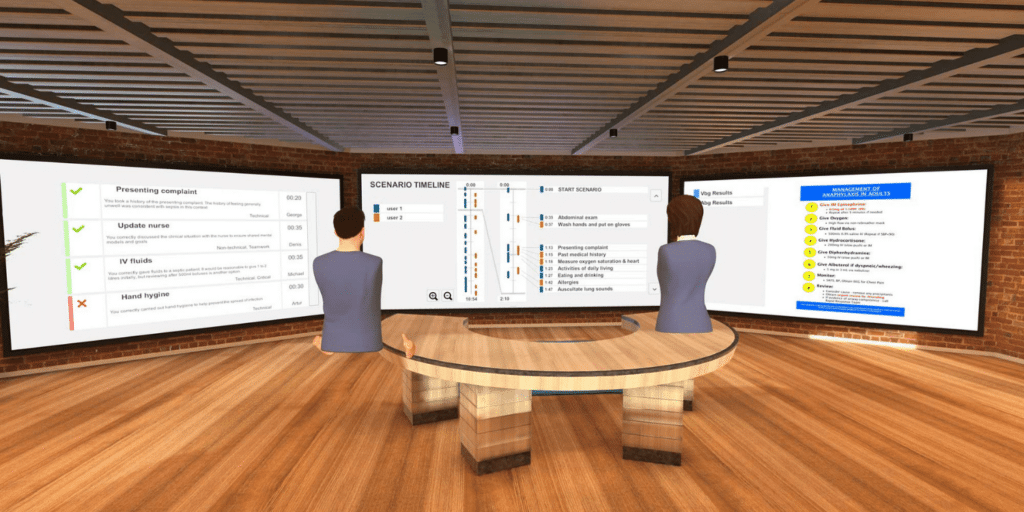
Self-guided questions that immediately follow a completed scenario challenge learners to think deeply about the case, giving them space to self-analyze and review feedback prior to debriefing in a larger group.
Between self-guided questions and automated, evidence-based feedback, each time a learner runs a scenario with OMS, they’re getting two of the three marks that the Healthcare Simulation Standards of Best Practice includes in their guidelines.
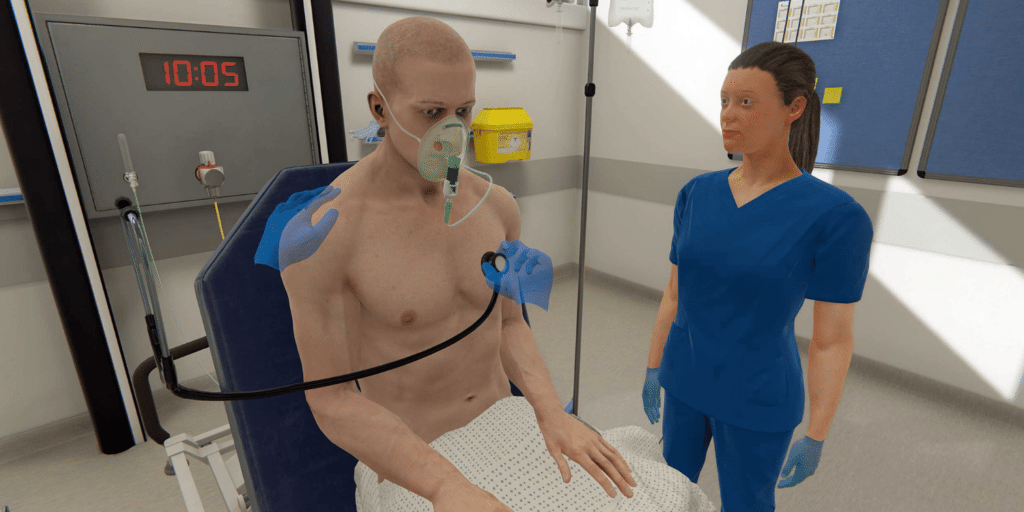
Beyond what’s provided by OMS, the context of the scenarios themselves make for rich debriefing discussions. Cases are authored by our team of in-house Clinical Authors to be true-to-life with virtual patients having robust narratives, and providing you with plenty of content to discuss within a group.
For instance, you may want to ask learners to talk more about which members of their interdisciplinary team would be helpful to speak with about a complex case and discharge planning. Or you may have deeper discussions about patient and family education or how work and life stresses may impact someone with a chronic condition.
Learners can use these types of prompts to further analyze a scenario in a psychologically safe learning environment that allows them to openly discuss mistakes, ask questions, and brainstorm alternative solutions.
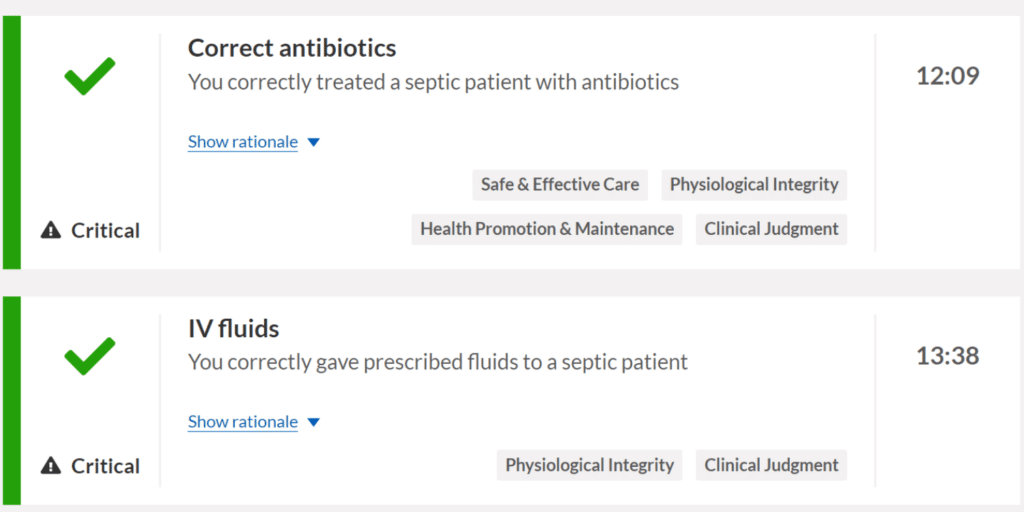
Automated feedback provides clear, evidence-based rationale for learners to more deeply understand the actions they took (or didn’t take), how they prioritized these actions, how they managed their time, and how they worked with their team. It also explains why these actions were important to the case, and how to improve for the future.
Creating a structured and productive debriefing session can require careful thought and planning, and OMS can help take some of that work off of your plate.
From pre-populated questions designed to initiate reflective thinking to cases with robust narratives that drive deeper discussion, OMS is here to support your learners in maintaining psychological safety while analyzing clinical performance.
To see what OMS has to offer for you and your learners, set up a demo with us here.