July 24, 2023
post
Clinician Decision Making in Virtual Simulation
Healthcare professionals, like nurses, doctors, or occupational therapists, make an incredible number of decisions per day. In fact, nurses working in critical care actually make decisions almost every 30 seconds, adding up to about 960 decisions made in a single shift of work.
Healthcare professionals, like nurses, doctors, or occupational therapists, make an incredible number of decisions per day. In fact, nurses working in critical care actually make decisions almost every 30 seconds, adding up to about 960 decisions made in a single shift of work.
This inordinate amount of decision-making directly impacts patient care, so it’s vital that clinicians are not only making and acting on these decisions but also that they’re taking into account a multitude of factors given the context of the case to make the best possible decision for their patients.
In order to build a skill, even complex and nuanced ones, repetition is a key component of success. Healthcare professionals and students alike need to continually leverage the knowledge they have to apply their skills and put it all together to make sound clinical decisions, and the use of new digital tools is one way to allow for consistent and flexible repetition to maintain or build skills.
Clinical Decision Making
There are lots of terms used to describe a part of the whole process of making a clinical decision, and while they are all a piece of the puzzle, they’re not necessarily interchangeable.
The term ‘clinical reasoning’, for example, was studied in a scoping review which found that across several hundred papers across health professions, 110 different terms were used to describe or to reference the concept of clinical reasoning.
Within the context of physical or occupational therapies, there are explicit definitions in clear frameworks that use this term to describe the process of clinical reasoning, however, not all disciplines use the same definition or frameworks.
‘Clinical judgment’ is a term becoming more quantifiable thanks to the National Council of State Boards of Nursing (NCSBN) who created a working model to measure clinical judgment in the Next Generation NCLEX.
There are several models or frameworks used to describe the process of clinical decision making in nursing, and there are multiple factors that can influence the decision-maker, both intrinsic to the decision-maker, e.g. experience level, and extrinsic, i.e. environmental factors.
Clinical decision-making is context-dependent and often time-sensitive, meaning all of the factors that go into a decision and action require high-level cognitive skills to efficiently assess and analyze the entirety of the situation, then form a judgment, make a decision, and act.
Methods like simulation-based education have been used to bolster the connection between theoretical knowledge and practice, and as virtual reality has been adopted into the healthcare industry, it’s gaining more traction in its use for the development and assessment of harder-to-test concepts like critical thinking, clinical reasoning, and clinical decision making.
Virtual Simulation Supporting Clinical Decision-Making
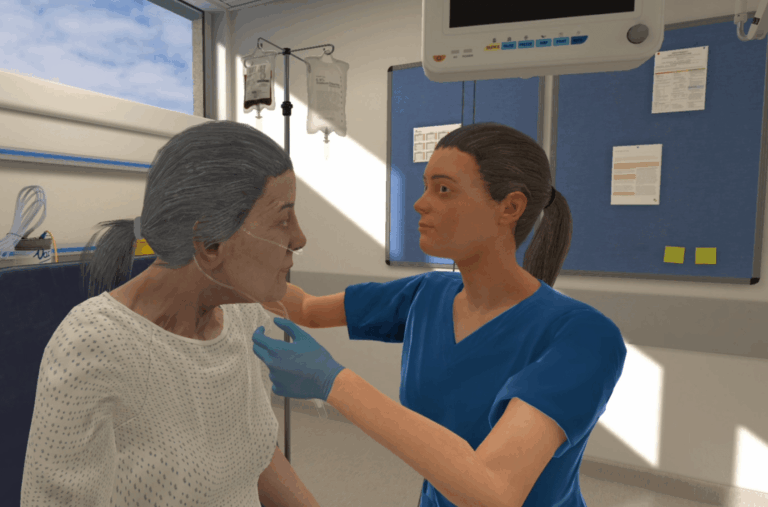
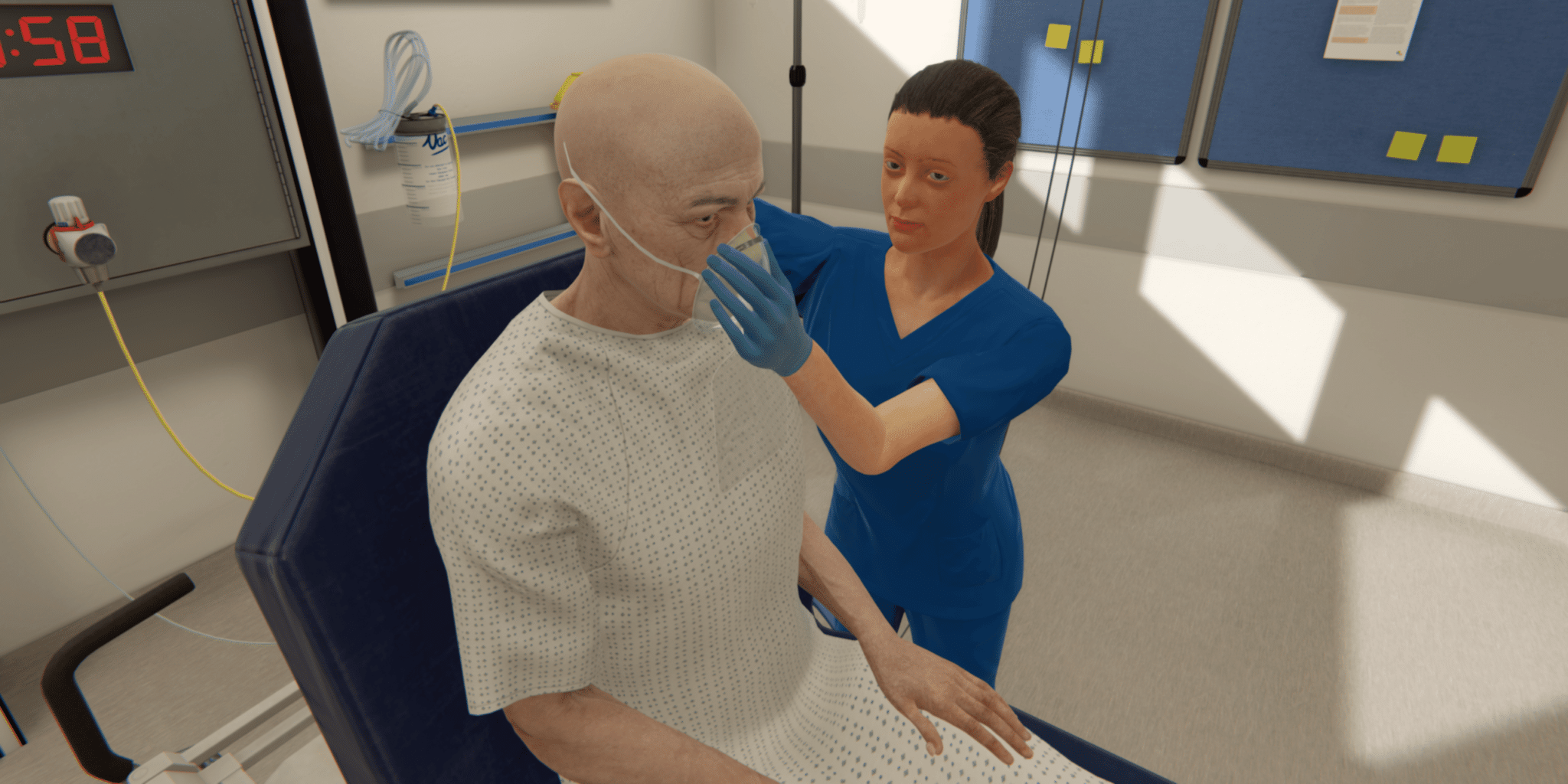
Virtual simulation, often used as an umbrella term to include in-headset & immersive virtual reality (VR) and virtual screen-based simulation (VS) has become an accessible and flexible way to have learners work on skills and knowledge transfer in and outside of the classroom or clinical setting.
A systematic review spanning 1996-2018 found that 86% of included studies reported that virtual simulation had a positive effect on students’ learning outcomes, which included critical thinking and decision making, as well as knowledge and skill performance, among others.
For undergraduate nursing students, in particular, virtual simulation has been used to bolster the development of clinical decision making skills, and while more extensive research is needed in this rapidly-evolving field, virtual simulation appears to be promising for cognitive skill-building in future healthcare professionals.
Virtual simulation offers a means by which learners can engage in simulation-based education at any time, anywhere, with unlimited opportunities to repeat and practice skills at their own pace.
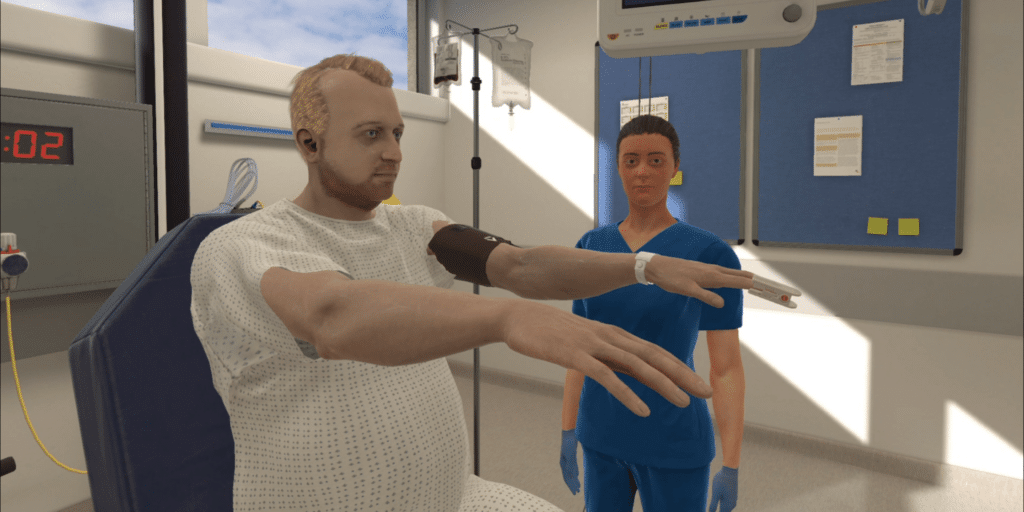
As virtual simulations are standardized, they’re able to be used to both practice conceptually-driven skills like clinical reasoning and for procedural skills like catheterization.
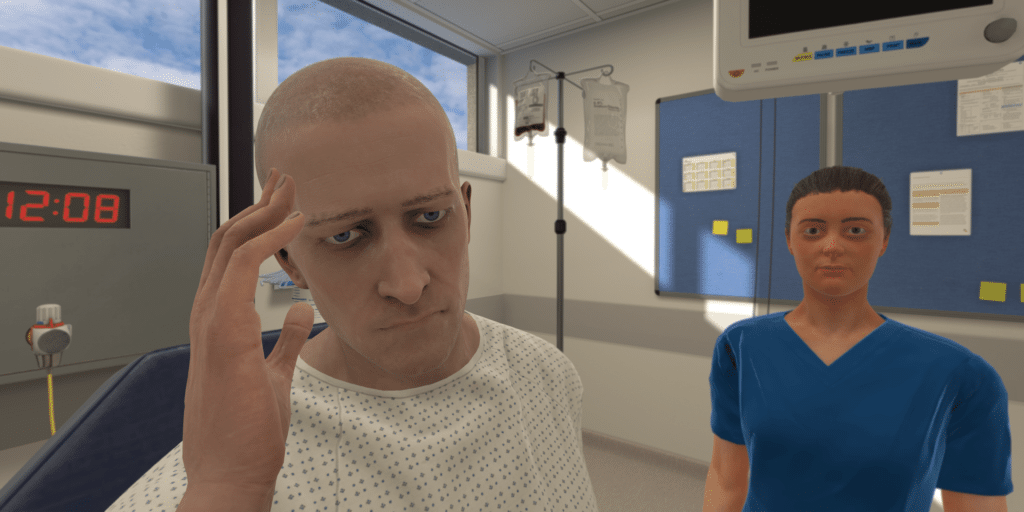
By placing learners in a lead role, it’s easy to see how virtual simulation can encourage and challenge cognitive skills like clinical reasoning and judgment.
In these scenarios, learners can assess the situation and gather relevant information through a variety of methods and use context-dependent reasoning and observational skills to inform hypotheses and implement interventions without ever placing patient safety at risk.
Learners are ablze to practice making decisions in a timely manner in a safe environment where mistakes are encouraged and used as a learning opportunity.
Automated feedback can reinforce well-understood concepts and skills while providing the evidence-based rationale to bolster acquired knowledge and bridge the gap for skills or concepts that prove difficult to transition to practice.
In addition, virtual simulations can be used to assess these types of skills – University College Birmingham has utilized VR in this way with plans to expand its use in their programs, and Stamford Health has used VR to assist their entry-level nurses in the transition to practice.
Virtual simulations continue to show promise for their use in the development of skills like clinical reasoning and decision-making. To learn more about implementing VR into a curriculum or training program, set up a time to discuss it in more detail here.
Related
Ready to get real?
See how OMS can help your organization build confidence, competence, and clinical readiness for today’s healthcare.