Bringing realistic clinical simulations to life is no small task. Anyone who has been a part of a simulation day knows a thing or two about all the work that goes into it. So many decisions need to be made, schedules need to be aligned, and skills need to be developed – all in such a short time.
With simulation-based education, learners can practice skills through a range of modalities, whether it’s working on suturing skills with a task trainer, practicing history taking with a simulated patient, or leading a patient case in virtual reality.
As technology continues to rapidly evolve, it has become further embedded into training programs and curricula, providing immersive and experiential learning opportunities for current and future healthcare professionals.
These immersive experiences are often grouped under the umbrella term, extended reality (XR), which includes augmented reality (AR), virtual reality (VR), and mixed reality (MR).
AR, VR, MR - what’s the difference?
As immersive technologies like AR, VR, and MR have become more widely implemented across the healthcare continuum, there has been a call to the community for clarity of definitions.
While extended reality is the umbrella term, there are significant differences between modalities.
Broadly speaking, augmented reality blends the digital and the physical worlds, creating a learning experience with both real-world and virtual elements.
Mixed reality, however, involves elements of both the physical and digital worlds, and learners here can interact with both worlds. This is different from AR, as learners in AR can only interact with the physical elements of the environment, even with the digital component present.
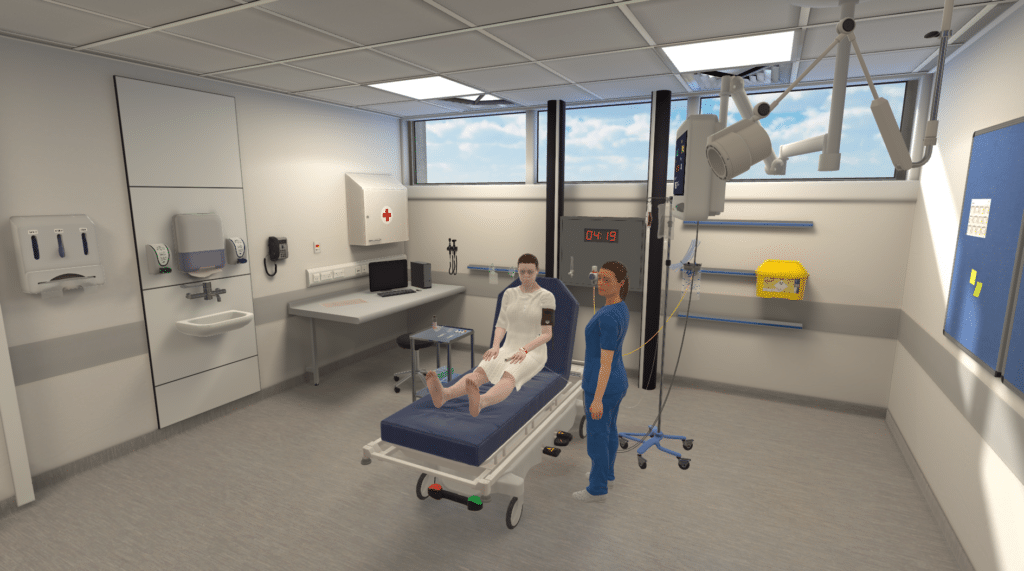
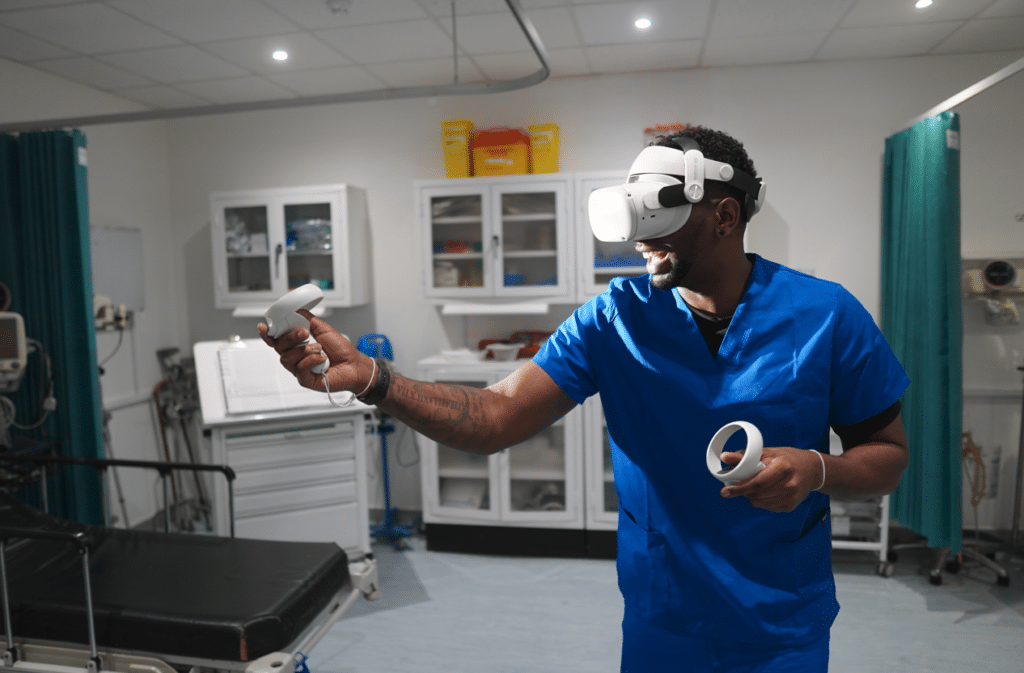
Virtual reality recreates elements of the physical world in a virtual environment. With a head mounted display (HMD), learners can become completely immersed in a virtual world, wherever they are.
In short:
- AR – uses the real world with the addition of digital overlay
- MR – blends the physical and virtual, where learners can interact with elements of both worlds
- VR – learners are fully immersed in a virtual environment, able to interact with elements of that environment
AR, VR, and MR in healthcare education & training
As selecting any simulation modality goes, it largely depends on the learning objectives.
Elements of surgical procedures can benefit from using augmented reality for skill transfer. For example, practicing suturing skills on a task trainer is a form of simulation, but if you were to add a digital layer displaying the steps of the procedure, that would be referred to as augmented reality. In AR, learners can physically perform the procedural skills with digital information contributing to and enhancing the learning experience.
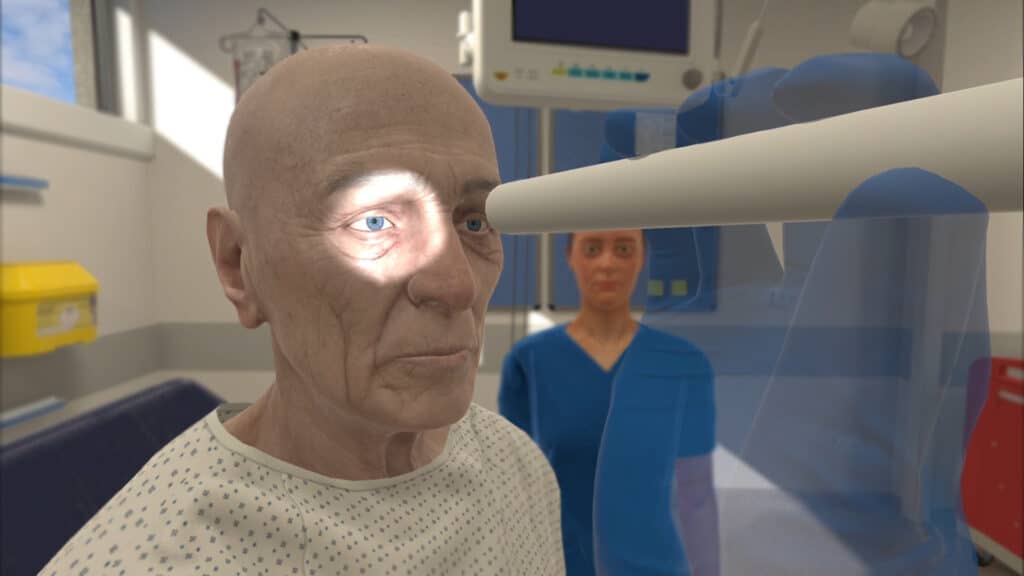
One example of mixed reality in nursing education is a study in which participants performed a visual assessment of a holographic patient projected into a real-world environment. Here, learners had the opportunity to engage in observational analysis, or ‘noticing’, which has been linked to the development of clinical judgment.
Virtual reality, meanwhile, has been used in the development of a number of clinical skills, including clinical decision making and nontechnical skills. Often, learners immersed in these experiences must lead the simulation, emphasizing the importance of individual learning and critical thinking.
Benefits of XR technologies in curriculum
There are lots of reasons you might consider adding extended reality to complement or add onto learning experiences.
On the whole, XR technologies offer a standardization with training that can be difficult or impossible to achieve in physical simulations.
Head mounted displays or laptops increase accessibility and portability, meaning more simulations can be conducted, on a more individual basis, and in less time than other forms of simulation.
There’s also evidence demonstrating that the use of XR technologies can increase learner engagement and improve spatial representation, and have been shown to positively impact skills, knowledge, and attitudes of the learners engaging in these types of simulations.
From a pedagogical perspective, XR provides experiential learning, placing the learner at the center. Learners can engage in situations from differing viewpoints, collaborate with peers, and can transfer knowledge to practice independently.
These technologies can prove especially useful in situations where clinical placements are limited or more specialized areas of care are not easily accessible.
Learners can access simulations remotely and gain exposure to areas of care they might otherwise never experience as a student or rarely experience as a practitioner.
VR, AR, and MR can provide opportunities for individual learning, emphasizing the application or development of skills like clinical decision making and encouraging deliberate practice and reflective thinking.
Selecting the best XR technology
Again, this largely depends on the learning objectives and what learners are ultimately trying to achieve.
Once learning objectives are established, a next step may be considering the level of immersion that would most benefit the learner.
Both MR and AR provide advantages for simulations that require an interaction with the real world.
For example, AR or MR may be better suited for skills like surgical equipment management, as learners can physically interact with objects they will use in the operating room.
However, in both AR and MR, learners continue to be limited by their environment. For example, practicing skills in MR in the living room may inhibit a sense of presence or realism, as the learner remains aware that they are actually in a room of their home rather than a clinical setting.
Virtual reality, on the other hand, promotes immersion and presence by placing the learner directly in a 360 degree virtual environment.
In VR, learners can be anywhere – whether it’s a hospital room, outpatient clinic, or home health setting.
Not only can a higher level of immersion increase the realism a learner experiences during the simulation, it has also demonstrated significant increases in knowledge retention for learners.
Additionally, virtual reality provides a distraction-free environment by blocking out the real world and leaving the learner fully immersed in the virtual space. Once in the simulation, the learner can engage in and lead the session independently, receive and reflect on feedback, and repeat the simulation as much as needed to bolster clinical skills.
For scenarios that are dependent on the environment – home health, for example – VR is the only XR technology that can bring the learner completely into another space and allow them to interact with virtual equipment, patients, or caregivers.
Overall, XR technologies can provide a safe learning environment where learners are free to make mistakes, reflect, and learn from them, and authentic, evidence-based scenarios can provide more standardization with training and tracking progress in competencies.
As the authors of a study on XR in medical education concluded, “the research question these days is not whether XR is comparable or even superior to traditional media for medical education, but where and how it should be deployed for maximum impact.”