April 20, 2023
post
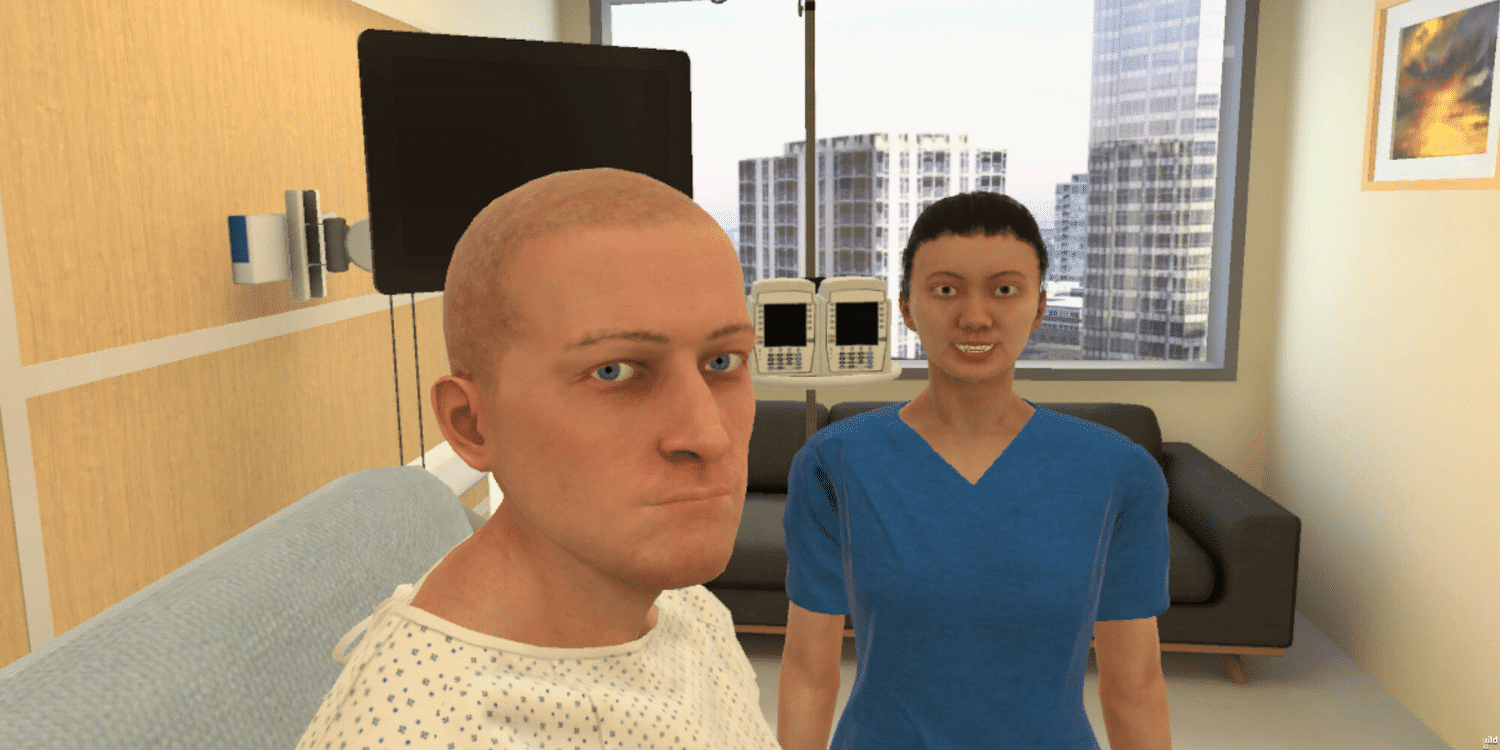
Multi-Patient Scenarios: A Next Step in Preparing for Practice
In the United States, recent data has shown concerning rates around readiness to practice. With 91% of assessed new-graduate nurses landing outside of the acceptable range of competency for novice nurses, it’s crucial that students preparing to graduate have realistic experiences that reflect the daily responsibilities of clinical practice.
In the United States, recent data has shown concerning rates around readiness to practice. With 91% of assessed new-graduate nurses landing outside of the acceptable range of competency for novice nurses, it’s crucial that students preparing to graduate have realistic experiences that reflect the daily responsibilities of clinical practice.
Creating true-to-life simulations is an involved process, often requiring significant planning, scheduling, and coordinating to achieve.
Scaffolding simulations – or scenarios that build upon one another and maintain continuity – is no easy feat, and then there’s the matter of tracking actions and providing objective feedback to learners.
As a way to begin to address the gap in knowledge from graduation to clinical practice, OMS has created multi-patient scenarios, giving learners the opportunity to use their clinical reasoning, delegation, and prioritization skills, all while simultaneously caring for other patients.
What are multi-patient scenarios?
Multi-patient scenarios are a set of simulations that build upon one another, allowing a single learner to incrementally increase their caseload.
The first scenario in this set runs just like any other – a single player assumes the role of practitioner, assessing and providing care to one patient.
The following scenarios each introduce an additional patient, corresponding to their number in the set. For example, the second scenario will have two patients, the third will have three patients, and so on up to five. Not all patients will require direct care, so you’ll need to coordinate by other means, e.g. over the phone or by delegating tasks to others.
As the simulations progress, you’ll manage more patients at various stages of their stays. Some patients have only just been admitted while others are progressing towards discharge, and because these simulations maintain continuity, you’ll get a chance to follow one or more patients during the course of their hospital admission.
You may also receive information about other patients from team members during the scenario. You’ll need to interpret their reports and use your clinical judgment to make in-the-moment decisions around what to do or who to see next – and the urgency with which you’ll need to respond.
How can you use these scenarios?
These scenarios are designed to challenge prioritization and delegation skills by requiring you to manage a growing caseload with increasing complexity. As you take on more patients, you’ll need to manage the cognitive load that comes along with those responsibilities. You should be prepared to answer questions about your patients, interpret findings, make clinical decisions, and manage related tasks all within the allotted time.
Beyond what you address within the scenarios, you’ll find plenty of topics that make for rich debriefing discussions. Using the context of the cases, more robust conversations can be had around points like environmental safety, social supports and discharge planning, interprofessional communication, and the role environmental stressors can play in patients with chronic conditions.
The standardized nature of OMS scenarios also means automated, evidence-based feedback with rationale. With the Competency Mapping & Tracking feature, you’ll also be able to view the actions taken in scenarios that align with competency frameworks like the NCLEX.
These scenarios can be used for training purposes, as well. You can also use this set to make decisions during the recruitment process or have employees complete these scenarios as a part of their onboarding or continued training, particularly in areas like quality and safety. They may be especially useful for new graduates working to transition from graduation to clinical practice.
If you’d like to make these scenarios more or less complex, you can utilize the no-code authoring platform, OMS Create, to make adjustments to existing scenarios (or build your own from scratch).
To learn more about our multi-patient scenarios, get in touch with us here.
Related
Ready to get real?
See how OMS can help your organization build confidence, competence, and clinical readiness for today’s healthcare.





