Blog
How can you scale up simulation by leveraging technology to enhance student learning? The team at the Norwich University School of Nursing in Northfield, VT
Explore all blog posts
How can you scale up simulation by leveraging technology to enhance student learning? The team at the Norwich University School of Nursing in Northfield, VT
Each year, nurses are required to complete competency assessments or take part in programs that confirm their ongoing knowledge and skill development in patient care.
Putting on a virtual reality headset and diving into an interactive game or experience, like riding a roller coaster, can be a great way to
At OMS, we have always been committed to creating the most realistic learning experiences for our clients and learners. With advancements in AI technology and
Acuity levels often refer to a patient’s status level, with higher acuity meaning a more unstable condition. Sepsis is one example of a condition with
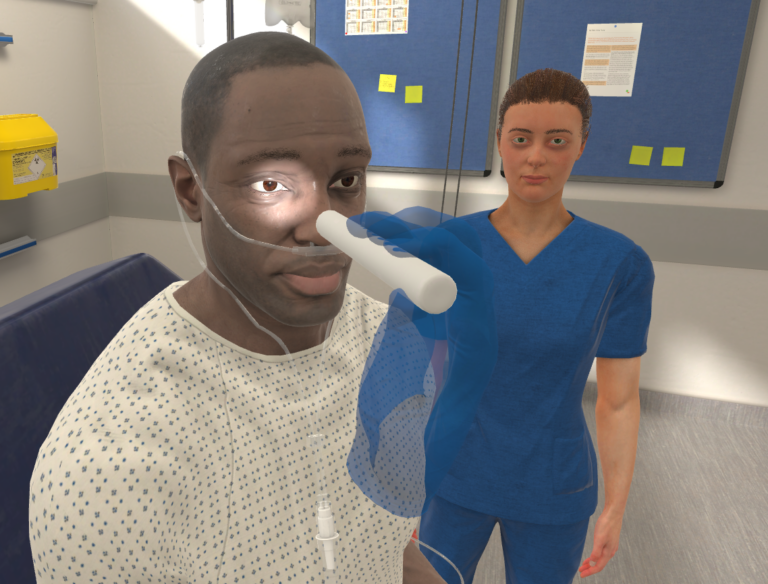
When it comes to healthcare training and education, simulation is a core component designed to apply, test, and refine clinical skills in a safe environment
What’s the deal with virtual reality? And why is it making such big waves? Maybe it’s time to pick up surfing and come along for
In September of this year, we hosted a group of leaders from across the United States, inviting them to join us in San Antonio for
Time flies – and it seems like technology is advancing at warp speed. Children growing up with this new set of technology, like Chat GPT
As a student in her final year of medical school, Dr. Alice Jones was introduced to virtual reality during her clinical simulations. Little did she
New Brunswick, Canada is a large yet rural province. Finding ways to support the healthcare needs of rural communities is a key challenge for the
Running a sim lab is serious business! Imagine… You’re in charge of running and maintaining your institution’s simulation lab, complete with manikins, task trainers, and,