October 4, 2024
post
Simulation and Your Return on Investment
Running a sim lab is serious business! Imagine… You’re in charge of running and maintaining your institution’s simulation lab, complete with manikins, task trainers, and, at times, standardized patients. As part of your role, you must coordinate the schedules of all 200 nursing students and faculty for a day of simulation – not to mention…

Running a sim lab is serious business! Imagine…
You’re in charge of running and maintaining your institution’s simulation lab, complete with manikins, task trainers, and, at times, standardized patients.
As part of your role, you must coordinate the schedules of all 200 nursing students and faculty for a day of simulation – not to mention the medical school and allied health students and faculty who are also in need of hands-on practice in the sim lab.
Students are eagerly awaiting their time in the simulation lab, since they’re off to clinical rotations in the coming weeks, and they need as much practice in their clinical skills as possible before heading into their rotations.
With all of that in mind, what happens when you’re already over budget (or close to it), but your manikin has just broken down, and you need to repair it before it can be used in another simulation?
It’s impossible to predict everything that might happen in the lead up to a simulation day, but what if there was an easier way to deliver more simulation to students without the headache or stress of coordinating all those schedules and maintaining all that equipment?
What about…?
There’s lots of different ways educators can deliver simulation to their learners, and it doesn’t always happen in person.
However, hands-on training and practice are vital to the learning process and in clinical skill-building.
While elearning and textbook reading can be helpful ways to disseminate information, it doesn’t have the element of hands-on or immersion that many students need prior to clinical practice.
Standardized patients are one way educators support the clinical development of learners, but there are certain conditions or symptoms that standardized patients simply cannot reproduce on command, like clamminess or pallor.
There’s the added element of objectivity and standardization, which can be hindered if there’s variations in answers to questions or if there’s confusion around how to react to certain questions, tests, or hands-on examinations.
Meanwhile, educators are often coordinating all of this at once while trying to simultaneously observe and educate the student practicing the skill(s).
Checkpoints or elements can be mistimed or missed entirely, and all the different elements to attend to can limit the debriefing discussion with the student afterwards.
What about a modality that both allows students to gain autonomy in their practice while alleviating educators of administrative burden, and that provides objective, detailed feedback and data for both students and educators on clinical performance?

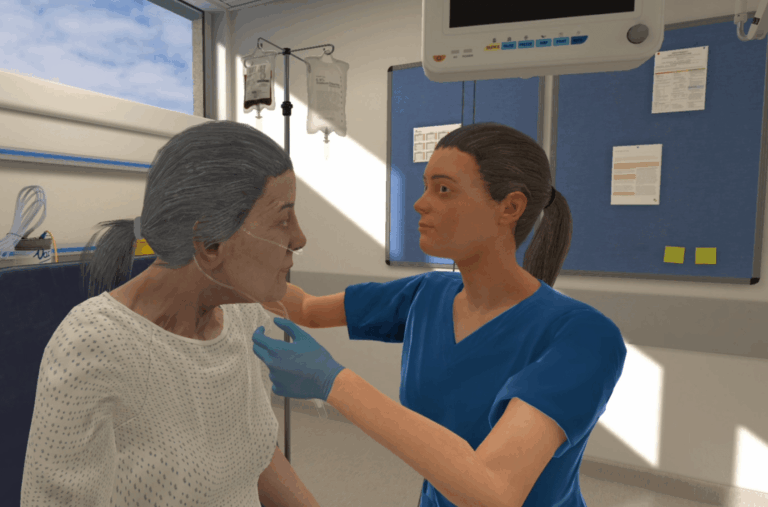
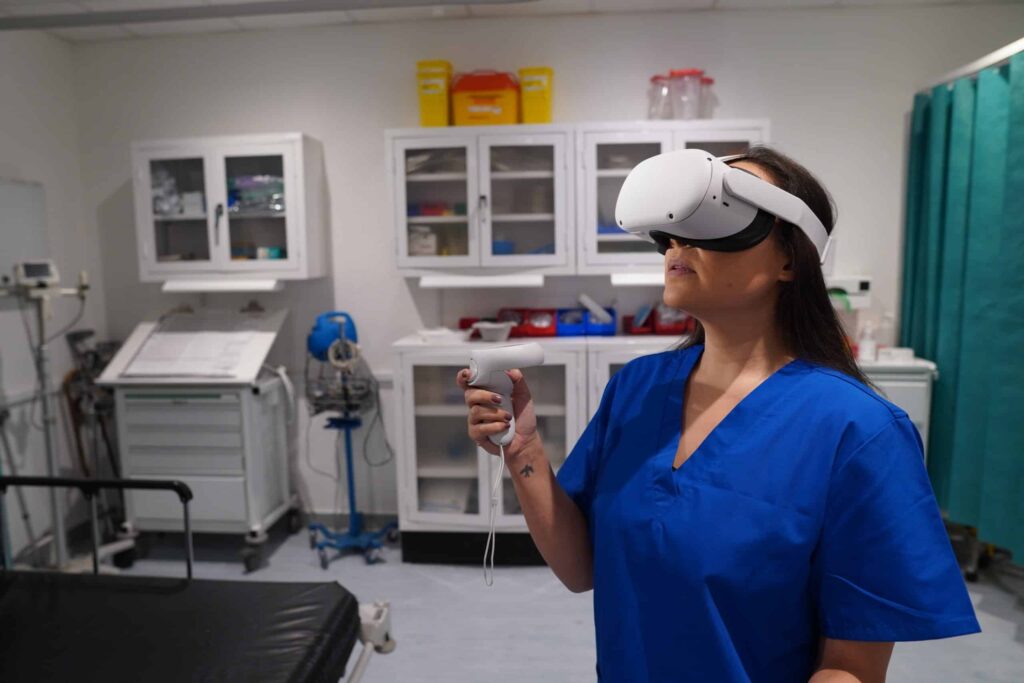
Enter: VR simulations
Practice makes perfect…or is it ‘perfect practice makes perfect’?
There’s something to be said about creating as realistic a simulation experience as possible for the learner while maximizing ROI for the institution.
Replicating not just the clinical environment, but also mimicking patient responses, observable signs of illness (and improvements) – even the background noise of a busy facility can all impact the learning experience.
While educators and simulation technologists are hard at work
Virtual reality can do all of the above, and it allows for endless repeatability and flexibility around how and when learners engage with simulation.
With VR, there come several benefits impacting ROI:
- Time savings
- Operational efficiencies
- Repeatability
- Space savings
- Scalability
Better flexibility means learners can conduct simulations on their own time and at their own pace – talk about deliberate practice!
This, in turn, means fewer slots scheduled for the sim lab space, freeing up educator and staff time while delivering more simulation. Not a bad combination.
Just take it from the folks at the University of Lincoln, who experienced a ‘drastically reduced’ workload and saved 200 hours of time in the sim lab using OMS.
Students at the University of Lincoln, like Kenneth Ward, feel “you can improve massively from VR”, with VR simulations leaving students like Francesca Ollier feeling “empowered and encouraged” at the end.
Michael Rowe, Associate Professor at the university, has said that using VR in this way “has made a massive difference to the way we think about assessment in this program.”
With a reduced need for space and scheduling, VR enables scalability in a way that simply isn’t possible with physical simulation.
The flexibility and accessibility of OMS means that VR can reach hundreds, if not thousands, of learners across multiple sites.
Saving time, reaching more learners, and providing more simulation opportunities is a significant stride in positively impacting both the learner experience and ROI.
The bottom-dollar line
Start here: using OMS resulted in a 74% reduction in staffing and equipment costs for Sheffield Hallam University.
Freeing up costs is a clear benefit to incorporating VR, and with significant time saved as well, educators can focus their attention on the critical component of debriefing and feedback for learners rather than the administrative tasks of simulation.
An Economic Impact case study by York Health Economic Consortium found that OMS costs were between $2.22-$14.38 per use, while physical simulation costs varied from $28.38-$394.95 per use.
Another study found that VR simulation requires 22% less time than physical simulation education and is 40% less expensive.
A cost-utility analysis concluded that VR delivers similar learning and performance outcomes when compared to physical simulation while being significantly less expensive.
When it comes to the bottom line, VR use can result in significant savings.
VR Effectiveness
Major cost savings are great! And while that’s all fine and well, will a new modality still improve learners’ outcomes?
Enter the evidence:
- Learners using OMS demonstrated significant increases in clinical confidence and performance improvement to Kirkpatrick level 3.
- VR significantly improved nurses’ knowledge over case-based learning, with higher levels of learning satisfaction.
- Evidence suggests VR improves healthcare knowledge and skills significantly more than in-person education or e-learning.
Of course, implementation of a new modality requires time, thought, and effort.
To get the most out of it, VR should be carefully aligned with learning objectives, course concepts, learner levels, and curriculum.
Luckily, at OMS, we can make that experience seamless with the curriculum mapping we provide as you consider how to best use VR for learners.
Additionally, educators must feel confident that learners are receiving up-to-date and evidence-based practice, and learners should feel confident in that, too.
Fun fact: At OMS, scenarios are created in alignment with Standards of Best Practice by Clinical Authors with professional experience in direct patient care, education, and simulation.
Scenarios also undergo a rigorous, 6-step peer review process to ensure quality and accuracy.
Repeated opportunities to perform skills in realistic, immersive, and evidence-based simulations can lead to significant improvements in confidence and competence for learners.
Students at the University of Lincoln reported, “you can improve massively from VR”, and “By the end of it, I felt really empowered and encouraged”.
And at the University of East London, faculty have said “Students are so immersed in these scenarios. They are highly engaged, and they want to continue learning more and more.”
This all together can help to boost support for learners while saving time, effort, and cost for educators and institutions.
What’s not to love about a system that brings fewer costs, time saved, and improved learning outcomes?
To learn more about how the OMS platform can help you meet your objectives, book a demo to speak with an Educational Specialist.
Related
Ready to get real?
See how OMS can help your organization build confidence, competence, and clinical readiness for today’s healthcare.