Be the provider, ahead of time.
Prepare for practice with VR sim.
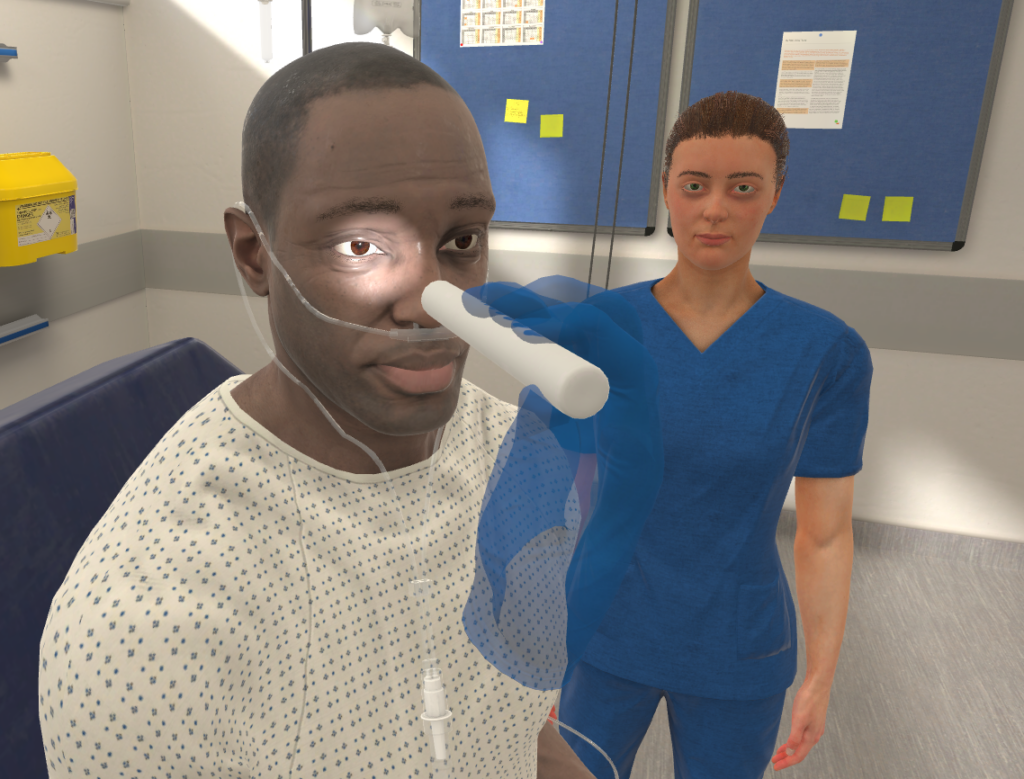
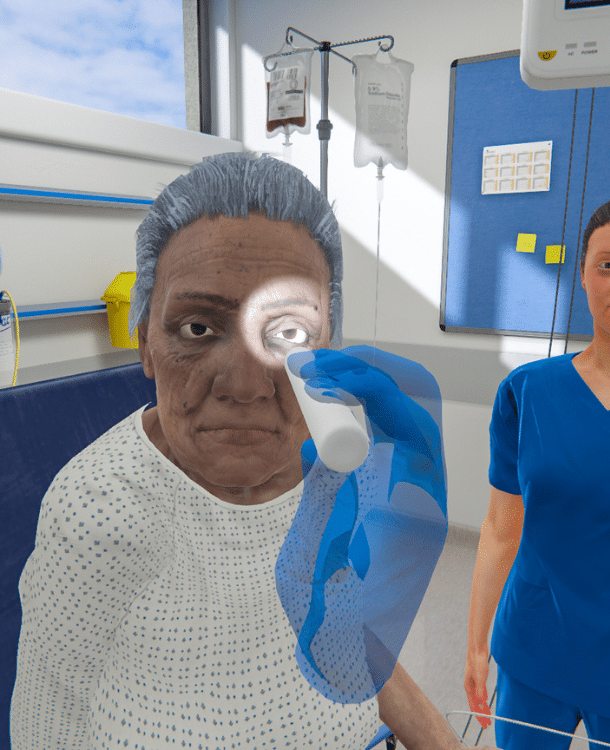
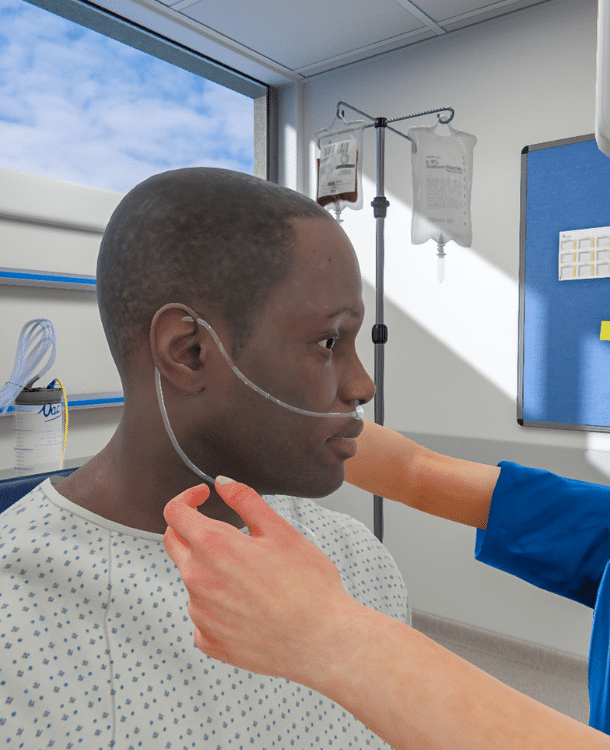
Enhancing clinical and diagnostic reasoning skills through immersive VR medical simulations.
What is VR simulation for medical education?
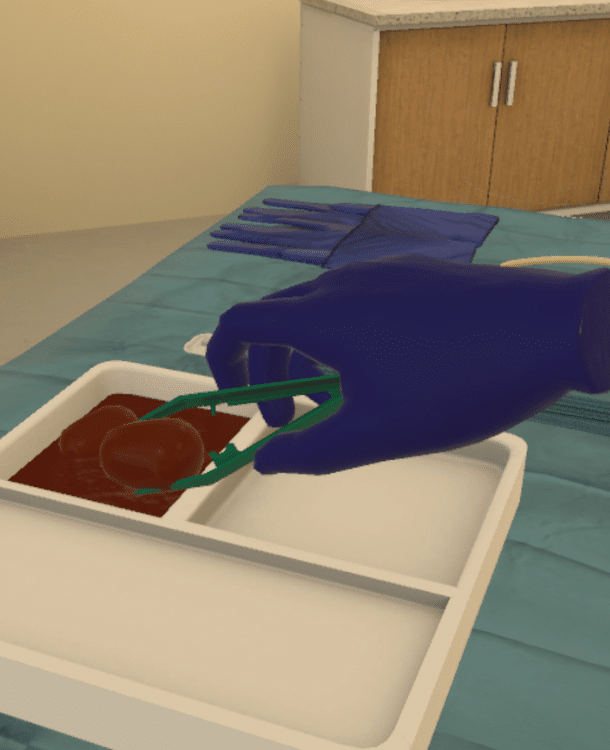
- An immersive, interactive, and engaging modality for competency-based medical education
- Allows learners to lead patient cases, reinforcing key skills like critical thinking, diagnostic reasoning, prioritization, and communication
- Complements didactic learning by providing a place where learners can immediately put theory into practice
Benefits of VR in medicine.
Save time & costs, enhance patient care.

Reduce variation in care
Standardize training while personalizing the learning experience. Reduce variability in care, improve patient outcomes.
Save time for everyone
Reduce learner training time, getting skilled clinicians to the floor faster. Free up educator time to focus on bedside teaching.
Provide total flexibility
At home, in the clinic - let learners work at their own pace, wherever it works for them. Repeat as often as needed to master skills.
Reduce training costs
Save on equipment costs, maintenance, and kiss consumables goodbye! Continue the savings the more you use it.
Build skills, reduce costs
Prepare learners for practice while reducing time, effort, and equipment costs.
Why OMS?
On the unit, in the classroom, or at home – OMS you can take anywhere.

Dynamic, realistic VR medical simulations
- Scenarios powered by AI for adaptive and responsive simulations
- Underlying emotion and physiology engines create realistic interactions in a safe learning environment
Standardized scenarios, objective results
- Automated and objective simulations create a truly standardized learning environment
- Robust data & analytics provide unique insights into trends and alignment with competencies
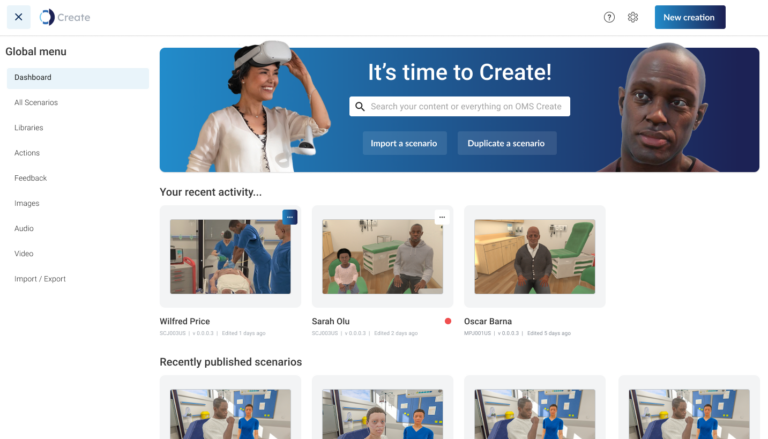
Intuitive authoring platform
- Edit from a library of over 250 existing scenarios across disciplines and specialties
- Change vital signs, feedback or scoring, or reconstruct the flow of a scenario
- Align scenarios with facility-specific protocols or guidelines to reduce variation in care
Frequently Asked Questions
Find answers to general questions around VR in nursing!
How is VR used in medicine?
VR medical simulations are used from the beginning of students’ education through the lifespan of the medical career.
Junior learners get practical experience before applying skills in the clinical setting, learning the role of the doctor and gaining real-world foundational skills they can use when they begin seeing patients.
Advanced practitioners get opportunities for repeated practice to stay fresh on their skills or learn new skills to advance their professional development.
What are the benefits of VR in medicine?
Simulation-based education is a cornerstone of medical education and training, however, it can be time and resource intensive to run a day of simulation.
VR medical simulations provide realistic and immersive sim experiences that can be repeated as much as needed, so learners can meaningfully apply skills in an immersive yet safe environment. More practice, more often can mean increased confidence, competence, and better patient outcomes.
Can two people be in VR at the same time?
Absolutely! With OMS, learners can conduct care individually or in team-based settings, so all the bases are covered.
When working in teams, learners can collaborate from anywhere in the world – whether they’re in the same room or continents apart, anyone can work together to practice team-based patient care.
What does VR simulation cost?
While price varies, adopting virtual reality in nursing can reduce time, equipment, and costs associated with simulation. One case study found that using OMS led to a 74% reduction in time and equipment costs compared to traditional simulation methods.
Other studies have shown similar findings, noting that VR simulation requires 22% less time and is 40% less expensive compared to physical simulation. A cost-utility analysis conducted by Haerling demonstrated the cost-utility ratio of virtual simulation to be $1.08 compared to physical simulation at $3.62 – the paper also found that while less expensive, VR ultimately delivered the same learning and performance outcomes as physical simulation.
Are there different ways to interact in the simulation?
Yes! Depending on the learner level and objectives, different modalities allow for various levels of interaction in the simulation.
For example, a communication-based scenario allows the learner and the virtual patient to have a real conversation, leaving the simulation very open-ended for learners to build communication skills. Other scenarios allow for menu-based interaction or more hands-on interactivity for procedural skills.
Are VR scenarios customizable?
All OMS scenarios are customizable through the no-code authoring platform, OMS Create. Common uses for the platform include: adjusting feedback or scoring, changing the level of difficulty, or changing the virtual patient’s physiology.
Scenarios can be made specific to an institution, allowing uploading of facility-specific information, documents, or protocols. Large changes, like changing the flow of a scenario or aligning one scenario with a different set of learning objectives, can also be done through OMS Create.
Those are just a handful of ways to tailor scenarios using OMS Create – the possibilities are endless!
Are OMS scenarios aligned with standards of best practice?
At OMS, scenarios are created by an in-house team of Clinical Authors who are clinicians, simulationists, and educators with a wealth of experience in healthcare education and direct patient care.
Clinical Authors use best practice guidelines to ensure alignment with standards of care, and all OMS scenarios undergo a rigorous peer review process to ensure a scenario is ready for release.
How will I be supported during the implementation process?
Rest assured that your OMS Educational Specialist and Customer Success representatives will work with you every step of the way to ensure a smooth transition process as you add VR into your program.
They will work with you from the early stages of curriculum mapping to collaborating on an onboarding and implementation plan, and they will continue to check in with you and provide support as you build out your VR program, well after you’ve started running your VR nursing simulations.
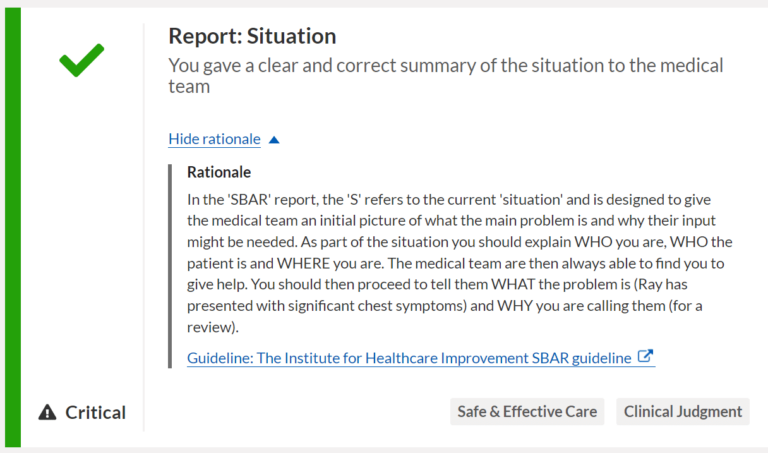
What data do learners & educators receive from the simulation?
The OMS platform is a comprehensive learning tool that logs and tracks data for both learners and educators.
Learners will receive immediate feedback following a scenario with areas of strength and improvements alongside evidence-based rationale.
Educators are able to access individual or cohort-based data to identify trends and remediate knowledge gaps.
With the Competency Mapping & Tracking feature, data can be even more specific, bridging theory and practice by logging actions taken in scenarios and aligning them with the core components of a given competency framework.
Are there VR simulations for any specialty?
With over 250 clinical scenarios (and counting!), the OMS platform provides access to scenarios across learner levels and specialty areas.
Libraries include VR simulations for areas including: maternal care, pediatrics, emergencies, community health, communication skills, procedures, and more – learn more about the breadth of OMS scenarios here.