January 17, 2024
post
The True Cost of Nursing Turnover: Why Nurses are Resigning and What It Means for the Healthcare Industry
Nursing has seen a shift in recent years that has caused alarm – higher turnover rates, staff shortages, and an increased demand for healthcare professionals have impacted the remaining staff and patients. It’s significantly financially costly for hospitals to replace lost staff, not to mention the time and resources cost of finding a suitable replacement….

Nursing has seen a shift in recent years that has caused alarm – higher turnover rates, staff shortages, and an increased demand for healthcare professionals have impacted the remaining staff and patients.
It’s significantly financially costly for hospitals to replace lost staff, not to mention the time and resources cost of finding a suitable replacement. With reduced staff and increased workload for remaining clinicians, patient care may also be negatively impacted due to turnover.
According to the 2023 NSI National Health Care Retention & RN Staffing Report, the average turnover rate has decreased by about 4%, now at an average of 22.5%.
A significant finding from the report, as RN turnover rate increases or decreases, with each one percent fluctuation comes a savings or cost to the average hospital of $380,600 per year.
Considering the average turnover cost of one RN has increased over 13% from 2021 – now standing at $52,350 – it’s apparent that improving staff retention continues to be a primary focus of the healthcare industry.
Why are nurses resigning?
The role of an RN is demanding, with significant pressures to perform at each stop, as patient safety is of the utmost importance.
While the role has evolved, there hasn’t always been such an urgency and need to retain current staff – so where is the gap, and why are nurses resigning today?
Of course, that’s a question with multiple perspectives and no one answer, but some data can provide insight.
As Oracle reports, nurses report that factors contributing to their decisions to resign include burnout, salary, and career advancement.
A 2022 report from the U.S. Public Health Service noted that burnout had already reached “crisis levels” even before the onset of the pandemic, as nearly ⅓ to ½ of nurses and physicians were reporting symptoms of burnout.
Staff shortages and an increasing workload on remaining nurses are another set of potential factors for this continuing cycle.
When too many staff leave, the remaining staff and patient care can suffer.
The remaining staff are often called upon to take on the additional workload, and patient-to-nurse ratios may increase significantly. At the same time, recruitment progresses, and nurses may need more individual time with patients.
Turnover rates for new nurses are exceptionally high, reaching up to nearly 40% of new hires leaving within the first year. This may be due to increased or unexpected workloads or a need for more structured support following onboarding.
This may lead to the overworked staff seeking a new role, retiring early, or leaving the industry altogether.
What can be done to increase RN retention?
As this is a multifactorial issue, a host of contributing factors need to be put in place to begin addressing and improving staff retention.
According to a McKinsey report, top factors that increase the likelihood that a nurse will stay in their role include a sense of doing meaningful work, an ability to rely on team members, adequate technology, professional development opportunities, and being valued by the manager and organization.
A lack of being valued by the organization was the most reported reason for nurses who decided to leave their roles. Staff support is a significant contributing factor, particularly for new nurses and recent graduates, and education and training is a central support component for new nurses.
Training often occurs in a simulation lab and requires advanced notice for scheduling purposes. Usually done in groups and, in many cases, during working hours that may otherwise be used for documentation or breaks, a simulation may only be run once or twice, significantly limiting the hands-on training for many of the staff present.
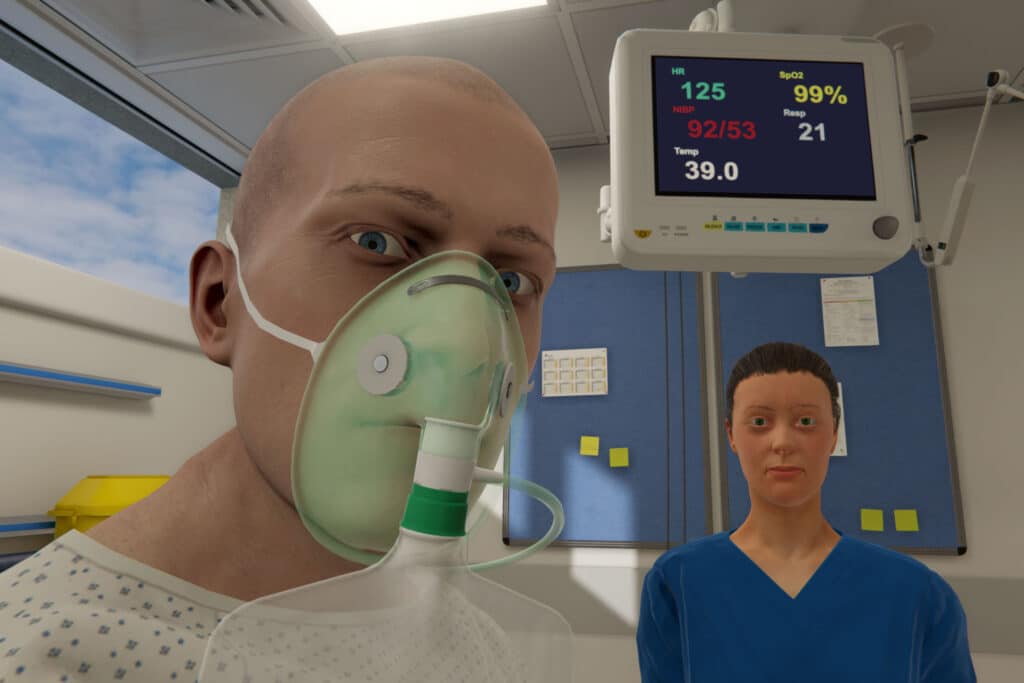
Some hospital systems have leveraged immersive virtual reality scenarios to enhance onboarding experiences, investing in staff training and helping them prepare for complex or infrequent, emergent clinical situations. A host of contributing factors must be implemented to address and improve staff retention.
Virtual reality and healthcare training
Bringing advanced technology into the fold can demonstrate to staff that a hospital system is invested in their career development and is working to bring meaningful and impactful learning experiences to a structured training program.
As many academic institutions have embraced VR, new graduates may expect healthcare systems to follow suit in providing access to state-of-the-art training platforms that help in their readiness and transition to practice.
In hospitals, virtual reality has been utilized to help in the management of diabetic emergencies, increasing learner confidence and improving their daily practice following VR simulation.
Reducing scheduling conflicts and providing more readily available access to simulation can mean that nurses have more opportunities for directed, deliberate practice and reflective thinking, creating more meaningful learning experiences focused on skills like clinical decision-making or communication.
Investing in staff training to support professional development and patient care initiatives can significantly impact both staff and patient care.
One hospital system, Carle BroMenn Medical Center, has leveraged virtual reality training to assist in the detection and timely treatment of sepsis. Since implementing their program, staff self-perceived confidence and competence improved, and performance scores across the hospital jumped by nearly 40%.
Accommodating the demanding work schedule of nurses and staff and providing access to up-to-date technology and meaningful learning opportunities may be one step to improving retention and ensuring healthcare professionals get what they need to perform at their best.
Related
Ready to get real?
See how OMS can help your organization build confidence, competence, and clinical readiness for today’s healthcare.





