August 23, 2023
post
Virtual Reality for Nontechnical Skills
Across industries, like healthcare and aviation, virtual, augmented, and mixed reality have been used to assess and progress technical and procedural skills from emergency medicine to pilot training.
Across industries, like healthcare and aviation, virtual, augmented, and mixed reality have been used to assess and progress technical and procedural skills from emergency medicine to pilot training.
As a result of VR’s growing use cases, research has expanded to include the use of these new technologies on the development of nontechnical skills, with a focus on skills like:
- Communication
- Critical thinking
- Teamwork
- De-escalation
- Empathy
- Situational awareness
According to a systematic review of virtual reality and healthcare professionals’ nontechnical skills training – teamwork, communication, and situational awareness were the most frequently studied nontechnical skills, which are often skills necessary for interprofessional teamwork.
These nontechnical skills, sometimes referred to as ‘soft skills’, are imperative not only for compassionate patient care, but also for the situational awareness and clinical decision making that comes along with the daily requirements of interacting with patients and making swift, sound clinical decisions at a moment’s notice.
Why use VR for nontechnical skills?
There are several emerging factors that indicate the use of VR as a valuable adjunct to healthcare education and training. VR can be a cost-effective way to promote reeducation or facilitate development of new skills, and it offers an added benefit of portability and requires minimal space to set up.
Another key feature of virtual reality simulation is the individualized practice that learners go through compared to other methods of simulation that often occur in groups.
Educators, trainers, or simulation technologists may gravitate toward virtual reality, particularly for difficult to simulate situations, like large-scale emergencies, or for conditions and situations that are not often seen in daily clinical practice.
As virtual reality can be engaged with remotely, it opens the door for members of interdisciplinary teams across departments to work together wherever they are, eliminating some of the administrative work of coordinating schedules or reserving a conference room.
A systematic review looking into the design of virtual patients in medical communication skills noted the strengths and areas of improvement for virtual reality simulation in medical education, and reported that VR remained an area of interest and promise, in part, due to the repeatability and immediate feedback provided by VR.
Specific nontechnical skills in VR
Patient Interactions
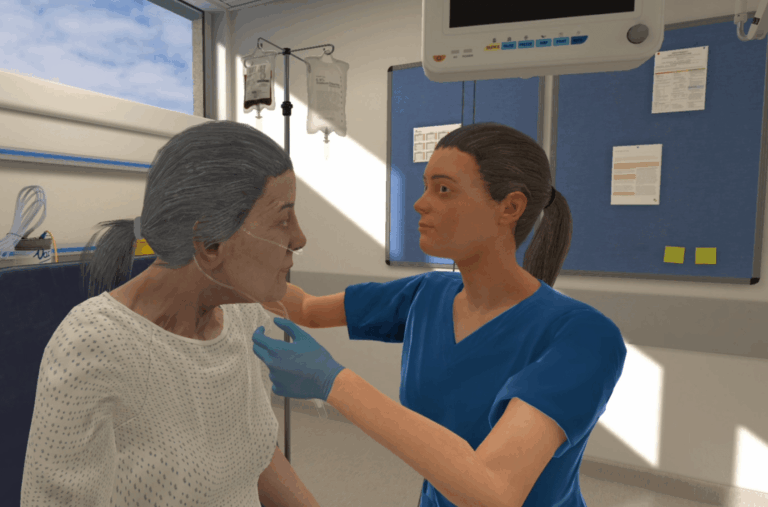
With AI becoming ever-more advanced, the use of AI-driven virtual patients allows learners to have conversations with patients in the VR world just like they would in real life. This use of voice control, combined with the rich backstories of virtual patients, brings an additional layer of complexity to virtual scenarios and allows learners to stretch their nontechnical abilities.
Particularly in scenarios focusing on complex communication, such as de-escalation, breaking bad news and motivational interviewing, skills such as communicating in an empathetic and holistic manner are vital – and VR allows this training at scale.
Interprofessional Teamwork
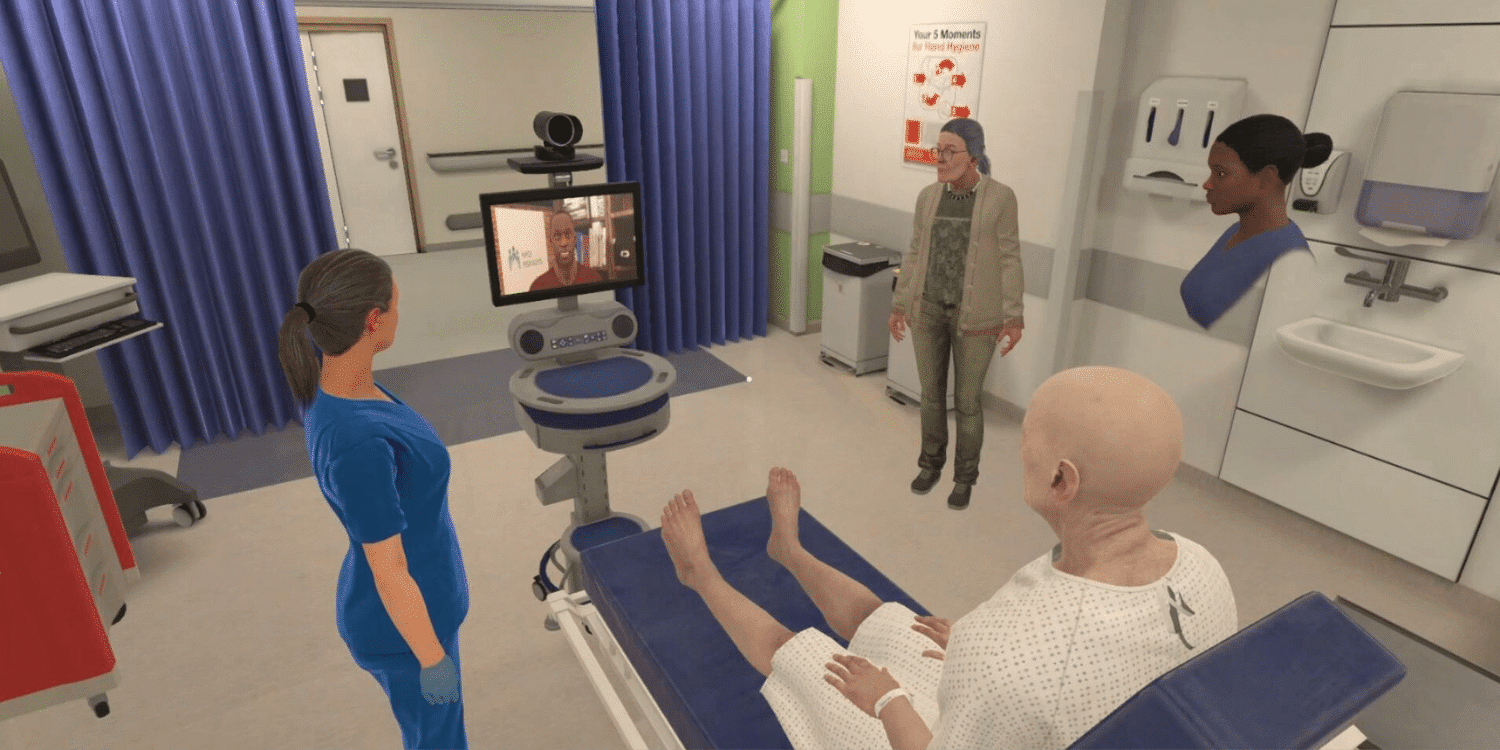
In many team-based scenarios, learners from multiple disciplines must work together to collect relevant information, form hypotheses, devise and conduct an intervention plan, and monitor the patient to determine the success of treatment or the need to make adjustments.
Learners can speak directly with one another during the scenario to facilitate timely team decision making and a collaborative interdisciplinary environment.
Additionally, interprofessional scenarios allow multiple disciplines to learn from one another, providing insights into the roles of other professionals, and with team-based feedback, learners can gain a deeper understanding of how their actions, and the team’s actions as a whole, impact patient care.
Clinical decision-making
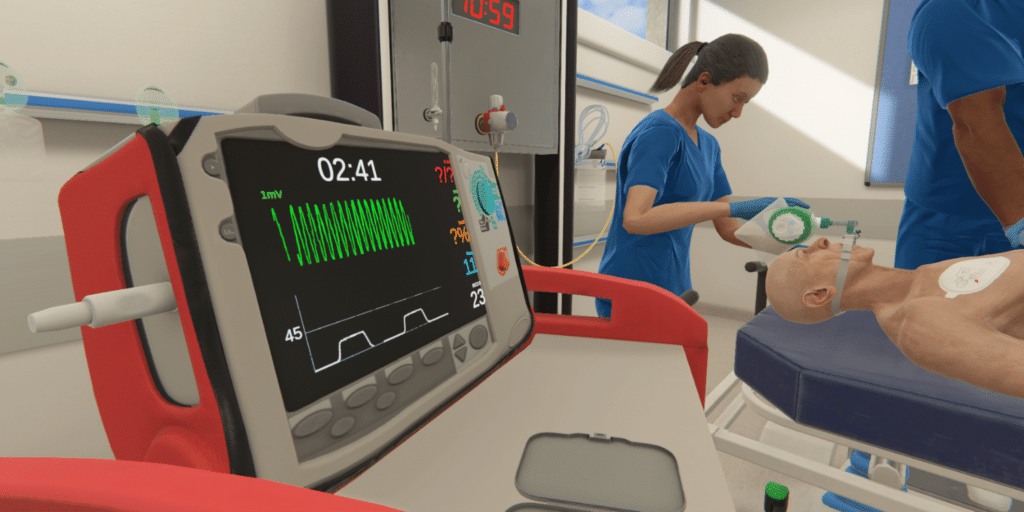
Independent of the type of scenario, learners can engage in critical thinking and situational awareness, informing their clinical reasoning and decision making skills.
By engaging in observational skills, learners can monitor patient status changes or fluctuations, like an onset of pallor or clamminess. Performing assessments, like vital signs or auscultation, can provide learners with pieces of information that help them put together a holistic picture of the patient’s status.
In taking on a lead role, learners become responsible for the collation of data provided by the patient and medical chart that, together, help to inform a clinical diagnosis. As this diagnosis becomes clearer to the learner, actions must be taken in order to address the underlying problem, meaning learners must know how to collect relevant information, interpret it, and how to intervene in the best interest of the patient.
The development of nontechnical skills is essential for both future and current healthcare professionals, which give clinicians a foundation from which to make appropriate decisions and communicate effectively, both interprofessionally and with patients.
The use of virtual reality for training nontechnical skills is a growing and exciting area of healthcare, demonstrating yet another possibility for using VR to supplement and innovate healthcare education and training.
Related
Ready to get real?
See how OMS can help your organization build confidence, competence, and clinical readiness for today’s healthcare.