September 14, 2023
post
Changing the Face of Education: Virtual Reality in Curriculum
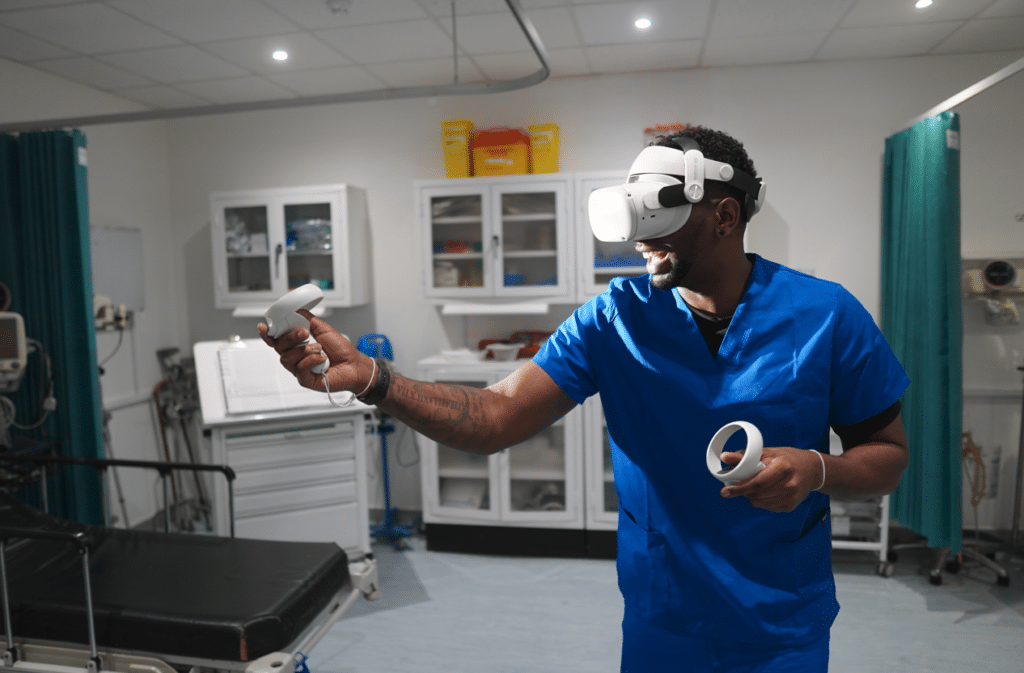
In healthcare education, students often must retain a hefty amount of information, and on top of that, they must build psychomotor skills they can take with them into clinical practice. Simulation is a well-known method to begin bridging the gap between knowledge and practice, and while it certainly has a place in healthcare curricula, it also has its limitations.

In healthcare education, students often must retain a hefty amount of information, and on top of that, they must build psychomotor skills they can take with them into clinical practice.
Simulation is a well-known method to begin bridging the gap between knowledge and practice, and while it certainly has a place in healthcare curricula, it also has its limitations.
Namely, physical simulation is resource-intensive. It requires significant planning, coordination, and it requires a lot from the faculty running the simulation, as well. There’s also the matter of finding an accommodating space and dedicating the time to execute an effective and smooth simulation.
To achieve similar outcomes at a reduced cost, virtual simulation can be a valuable addition to the teaching modalities used to hone and develop skills like clinical reasoning and decision making.
As is true of any progression within a curriculum, thoughtful and strategic placement of virtual reality can result in the best outcomes for both faculty and students.
Integrating VR into a curriculum
While counterintuitive, it may be best to start at the end – in other words, it’s important to begin with a firm understanding of the expected learning outcomes to determine where VR can best suit learners’ needs.
Scenarios should be matched to the learner level and, ideally, align closely with the didactic content of the course.
Authors at Johns Hopkins University did just that, and they created a roadmap with 4 areas of focus to define the optimal way to add virtual reality into a curriculum.
Orientation
The journey begins with an orientation process which should serve to familiarize both learners and educators with the platform they’ll be using.
Faculty can get an understanding of the scenarios and the data provided by the platform to give them all the tools necessary to leverage the VR experience.
Learners, in turn, get a chance to navigate the platform, and they’ll get the opportunity to navigate the scenario, as well. This way, learners can place their focus on the task at hand when in the scenario rather than on troubleshooting or setup.
Pre-brief
Next, a pre-brief can be used to get students in the right mindset before entering VR. In the case of JHU, they took this time to discuss concepts like psychological safety and confidentiality prior to beginning the virtual simulation.
Here, important concepts can give learners the background information or context necessary to optimize the experience. This can include anything from the rationale for virtual reality to reading materials to relevant information regarding the upcoming case.
As virtual reality can be engaged with remotely, it opens the door for members of interdisciplinary teams across departments to work together wherever they are, eliminating some of the administrative work of coordinating schedules or reserving a conference room.
A systematic review looking into the design of virtual patients in medical communication skills noted the strengths and areas of improvement for virtual reality simulation in medical education, and reported that VR remained an area of interest and promise, in part, due to the repeatability and immediate feedback provided by VR.
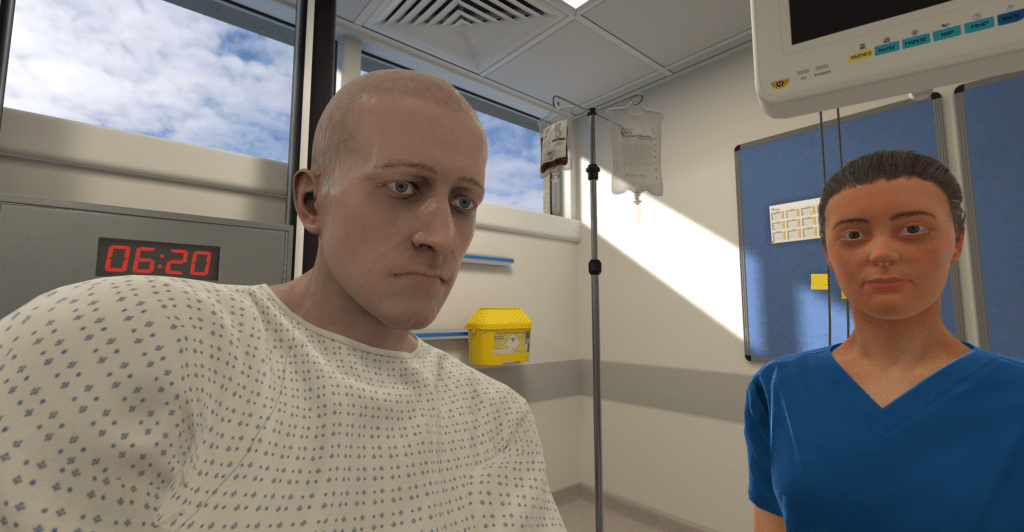
The Scenario
Once the pre-brief has been completed, learners can enter the virtual simulation and complete the case. It’s entirely up to the academic team to determine the length of time learners can access these scenarios or the benchmark score they must achieve in order to demonstrate meeting the learning objectives.
OMS scenarios take approximately 20 minutes to complete, and faculty can limit the amount of attempts learners may take; although, an ability to repeat as much as needed may be a benefit to more deliberate practice.
These types of decisions depend largely on the learning objectives and goals created by the instructors, which is another reason why beginning with predetermined goals can be so beneficial in choosing the right course of action in implementing virtual simulation.
Once learners complete the scenario, one of the most important components of simulation-based learning is next – the debrief.
Debrief
Debriefing is an opportunity to provide learners with feedback on their performance, which can make a big impact in overall learning. Traditionally, debriefing takes the form of synchronous, small group-based discussions, led by an experienced facilitator.
With virtual reality, this can still be the case. Additionally, scenarios may come with automated feedback, providing learners a chance to self-debrief before entering into a group discussion. Feedback with OMS is based on best practices and provides rationale to learners on concepts relevant to the case and appropriate actions to optimize patient care.
It’s important to take into consideration the perception of VR that learners have, so taking their feedback can help make decisions around the implementation of VR, as well.
Educators must also have their feedback considered, as they will be the people largely putting the time and effort into the initial curriculum mapping that takes place.
Adapting VR to your curriculum
Armed with your learning objectives, you’re likely to find a scenario that aligns with your needs in the OMS library of over 240+ scenarios.
However, if you’re not able to find what you need or if you’d like to make even the slightest of adjustments to an existing scenario, you can take the creation of the simulation into your own hands.
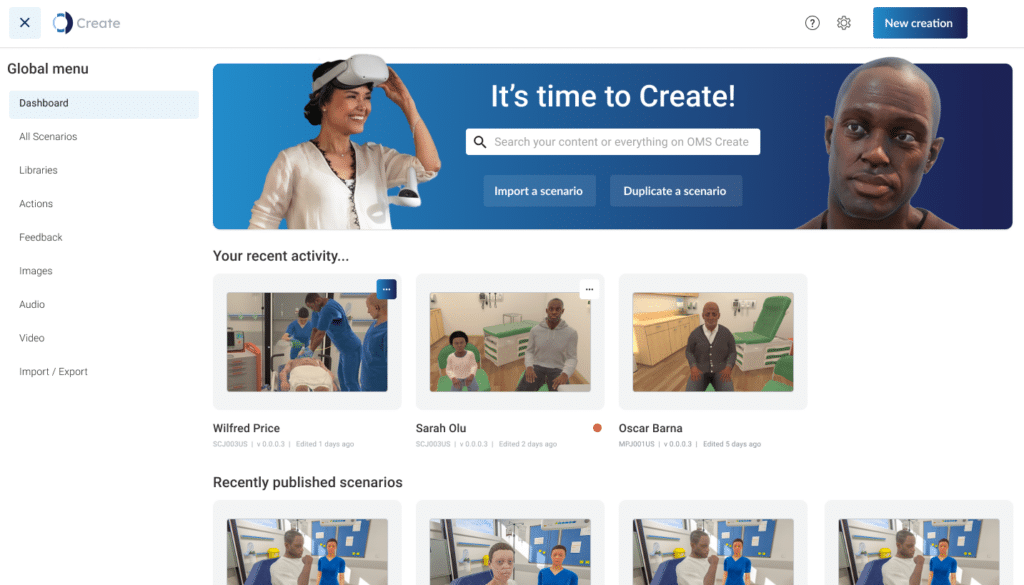
Maybe you’d like a vital sign to read differently or you need a virtual patient to have a different response – this can all be done via the no-code authoring platform, OMS Create, giving you the chance to make a VR experience that gives your learners exactly what they need.
Building, changing, and progressing a curriculum is no easy task, and it requires a lot of effort and planning to make it happen, but with the right tools and goals in mind, you can seamlessly add virtual reality into your curriculum to bring an innovative and informative teaching modality to your learners.
Related
Ready to get real?
See how OMS can help your organization build confidence, competence, and clinical readiness for today’s healthcare.





