Whether in the classroom or the clinical setting, opportunities for learners to practice skills freely and in a safe environment are limited.
However, replicating real-world clinical scenarios is crucial in preparing students for practice and reinforcing knowledge and skills for clinicians.
This recreation of specific clinical situations is often referred to as ‘simulation-based education’, and has become a cornerstone of nursing education and training.
What makes for a simulation?
Recently, the Nursing and Midwifery Council (NMC) updated their terminology to provide clarity on what constitutes a simulation, now considered “an educational method which uses a variety of modalities to support students in developing their knowledge, behaviours and skills, with the opportunity for repetition, feedback, evaluation and reflection to achieve their programme outcomes and be confirmed as capable of safe and effective practice.”
Several key features are listed in the NMC’s revised definition of what’s required of a nursing simulation.
While simulation may be delivered through “a variety of modalities”, it must be used to facilitate skill development and reinforce knowledge for students. Additionally, there must be an “opportunity for repetition, feedback, evaluation, and reflection”.
With this idea in mind, the NMC announced earlier this year that the changes enacted during the Emergency Standard for Nursing Education (RN6D) are now permanent, meaning that qualified institutions may provide up to 600 hours of simulated practice learning, counting towards the total requirement of 2300 practice learning hours.
For clarity, the NMC defines simulated practice learning (SPL) as a means to “replicate, support, and complement practice learning scenarios through a wide variety of methodologies”.
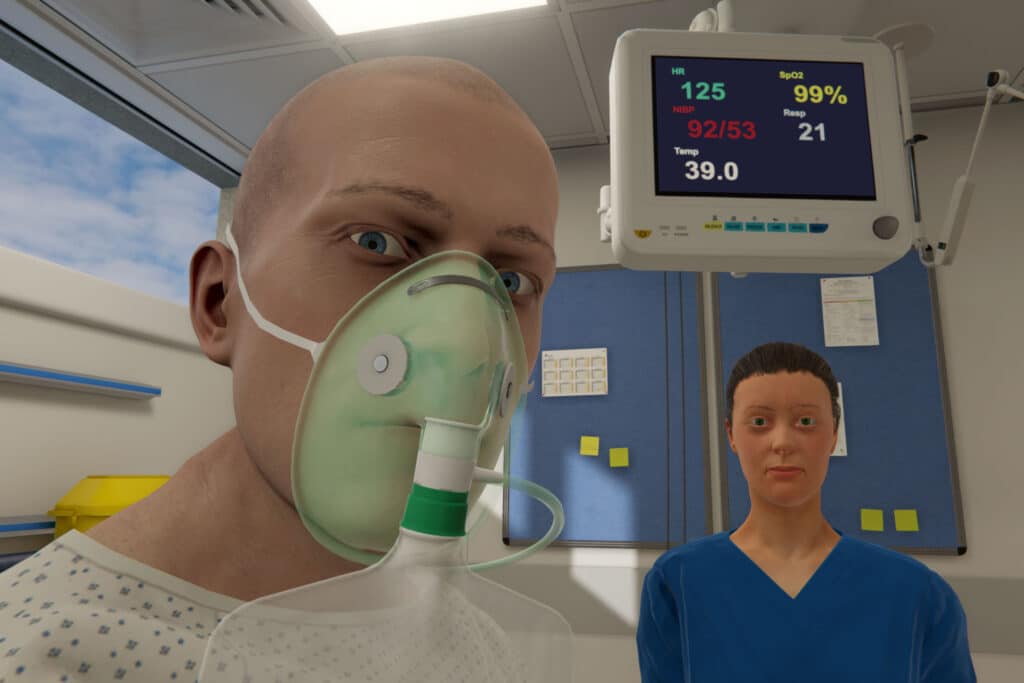
This might include working with standardized patients, immersive rooms, or virtual reality. There are additional requirements for what counts as SPL, including meeting standards previously set for pre-registration nursing programmes and demonstrating the achievement of learning objectives, among other requirements.
Simulation in nursing education
A recent study by the Council of Deans of Health (CoDH) looked at the whole of ‘Simulation in Nursing Education’, with findings supporting the use of simulation-based education in nursing.
Notably, the study reported that, consistently, simulation-based education “is more effective than traditional clinical education in improving outcomes such as knowledge, clinical judgment, critical thinking, and measures of clinical competencies”.
Interestingly, this study found that academic staff reported low confidence levels in using cutting-edge technology like virtual reality or augmented reality. This study also demonstrated low use levels for VR, AR, and on-screen simulation, indicating a potential need for familiarity with these mediums amongst academic staff.
This may also factor into reported requirements for successful implementation and maintenance of simulation-based education, including:
- Commitment from faculty leadership
- Access to space
- Funding and resources
Additionally, the “planning, delivery, and design” of simulations were seen as advanced skills for staff, potentially adding to the difficulty of implementing a comprehensive SPL into the curriculum.
Addressing challenges of implementing SBE
Common difficulties of physical simulation often include access to space or facilities, continuing cost of maintenance or equipment management, replenishment of consumable supplies, and scheduling conflicts.
Additionally, it’s often the responsibility of staff supervisors to observe students’ practice while running the simulation, track progress, and log relevant points that arise to facilitate meaningful debriefing discussions. On top of the cognitive load for staff, they may be responsible for the setup, reset, and breakdown of the simulation, which can become a months-long coordination effort for one to two days of simulation.
While manikin-based simulation or task trainers are ideal in certain circumstances, virtual reality is perfect for other outcomes.

For those seeking individualized training for a large cohort, an opportunity to safely assume a leadership role, or for the recreation of infrequent, high-stress situations that are difficult to replicate – these are just a few examples of the importance of using a variety of modalities when it comes to SBE.
Additionally, the CoDH study is one of many sources that find similar outcomes between virtual reality and physical simulation. A cost-utility analysis performed by Haerling also found “no significant differences in quantitative measures of learning or performance between participants in the mannequin-based and virtual simulation groups”. This study also reported a much lower cost-utility ratio favoring virtual simulation at $1.08 compared to manikin-based simulation at $3.62.
With VR, any space can be a learning environment. Quick setup, reset, breakdown times, and immersive, evidence-based clinical simulations make virtual reality a seamless adjunct to didactic learning and the transfer of knowledge to clinical practice.
As Brown et al. demonstrated in their paper on curriculum integration, virtual simulation can complement an existing program with positive student experiences.
Other benefits of virtual reality clinical simulations include ease of use, flexibility and accessibility, repeatability, and psychological safety.
Virtual reality has recently become a pivotal component of nursing education and training, and its use continues to rise, finding new avenues for adoption and use – for example, in Competency Mapping & Tracking or assessment.
With an easy setup, cost-effective maintenance, and the ability to recreate any situation, VR is an excellent addition to any simulation-based educational curriculum, allowing learners to direct patient care safely and providing immediate feedback and support for reflection and continued repetition of clinical skills practice.
For more information
For more on the benefits of virtual reality, see our research page, or to speak with an Educational Specialist about how best to integrate VR into your institution’s curriculum, set up a time to talk with us.
