As of April 1st of this year, the Next Generation NCLEX (NGN) is in effect!
That means new item types, cascading questions, and greater emphasis on critical thinking and clinical decision making.
These cascading questions involve a set of six questions, with a combination of different item types, that all relate to one case study. Test-takers will need to complete three of these case studies throughout the NGN, however, two will be scored while the third will be validated for future use.
An exciting time for many in the nursing profession, both in clinical practice and in education, it’s also likely to be somewhat daunting for the first waves of test-takers.
What is this new version of the NCLEX, and why should it be embraced, not feared?
Why was the NCLEX updated?
The National Council of State Boards of Nursing, or the NCSBN, noted the rising responsibilities of new nurses and the idea that they must make increasingly complex decisions during patient care.
This points to the expectation for new nurses to utilize clinical judgment, which is a concept that encompasses both critical thinking and decision making skills.
What’s more is that recent data has shown concerning rates in terms of readiness to practice. Of those assessed, 91% of new nurses were outside of the acceptable range for competency.
Another study reported that employers aren’t necessarily confident in their new nurses, either – in general, new nurses were viewed as underprepared to practice by their employers.
Given the association between poor patient outcomes and poor clinical decision making, the need to properly assess clinical judgment as a criteria for licensure has become even more pronounced.
Clearly, this concept of clinical judgment needed to be able to be reliably measured, and that’s one big reason why the Next Generation NCLEX was born.
A closer look
Of course, measuring a broader concept like clinical judgment is no easy task. It’s much different than measuring knowledge like general anatomy where much of the material is memorized.
Clinical judgment requires relevant knowledge and skills, and on top of that, it requires the cognitive ability to think critically and make decisions within the context of a given situation, sometimes in a very short period of time.
Therefore, following much research and consultation, a model on clinical judgment measurement was created.
Unlike other models, the Clinical Judgment Measurement Model is multi-layered, and importantly, layer 3 holds the key components of clinical judgment – which are also measurable.
They are:
- Recognizing cues
- Analyzing cues
- Prioritizing hypotheses
- Generating solutions
- Taking actions
- Evaluating outcomes
Layer 4 is also an essential part of the equation, as it acknowledges the different internal and external factors that can influence decision making.
Time pressures, task complexity, or distractions can impact how a decision is made, along with internal factors such as knowledge or experience level.
Therefore, it’s important to measure layer 3 while understanding the nuance of layer 4.
How are they measuring clinical judgement?
You’ve got an idea of the ‘why’ by now, but what about the ‘how’?
This overview from the NCSBN details just how these processes were developed and how new item types came to be.
There were numerous brainstorming sessions, writing panels, continuous review processes, drafts, rewrites, edits, and revisions, and ultimately, several new types of questions were decided on that ranged from the well-known to the brand new.
Classic item types like the standard multiple choice questions are still used. Other questions involve highlighting text or data, selecting all that apply, or selecting from multiple drop-down options.
Many of these newer types of questions increase the possible number of answer combinations, placing more emphasis on clinical judgment and critical thinking.
However, it’s important to note that there is opportunity for partial credit on some, but not all, types of questions. For instance, a wrong answer for a multiple choice question has no opportunity for partial credit while a wrong choice in a select-all-that-apply question may garner partial points.
These questions are often built upon one another, and several groupings may relate to one case, enhancing the realism of a written clinical situation.
For a given case, the first question may require identification of relevant case information, and the next item requires interpretation of those findings. For example, a question may ask for the most concerning finding(s) or which finding(s) require follow up or continued assessment.
As the case unfolds, new information will appear, requiring hypothesis generation and possible updating. These questions may ask about potential diagnoses or prioritization of problems.
Subsequent questions may ask about appropriate interventions and determination of the success of those actions. These types of questions revolve around the right types of interventions or medications, and understanding signs of worsening or bettering conditions.
These types of cascading, related questions are meant to more closely reflect the realities of clinical practice and following a patient’s case throughout the course of their stay.
How OMS can help in preparation
While clinical judgment is not a new concept, it is relatively new to being tested in a high-stakes, often pressure-intensive exam.
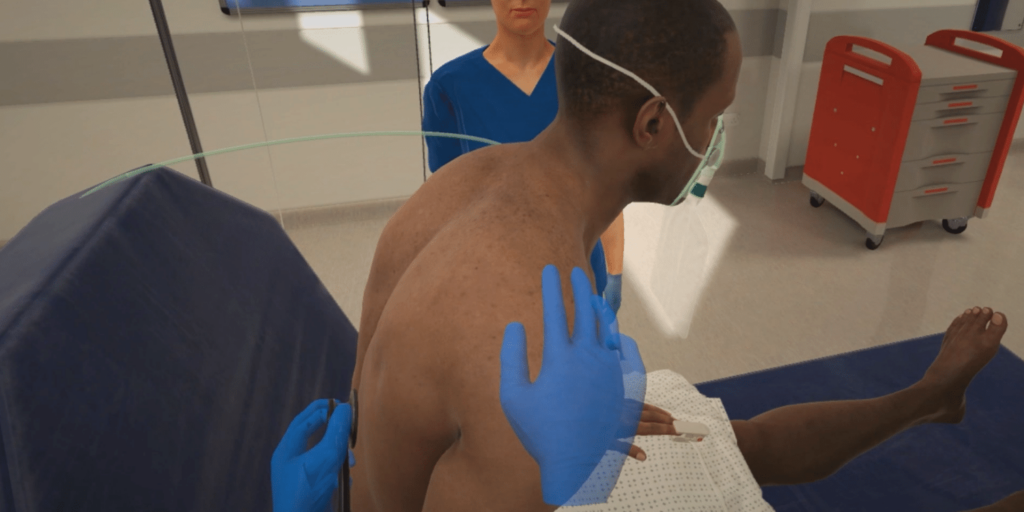
As you or your learners apply knowledge to practice, simulation is a wonderful medium to engage critical thinking and decision making under time pressure while remaining in a psychologically safe environment.
In many instances, swift and efficient information collection and analysis is critical for nurses to identify problems, determine the right actions, and commence interventions.
The authenticity of these scenarios mirrors actual clinical environments, embodying the inherent time constraints, distractions, and disruptions typically encountered throughout a shift.
As new information becomes available, learners must remain adaptable in their thinking, continuously filtering information and updating their current hypotheses.
For example, in OMS Multi-Patient scenarios, the learner may be interrupted in the middle of treating a patient with new information regarding a different patient, requiring attention, reprioritization, and delegation of tasks to accommodate it all in a timely manner and manage their caseload of multiple patients.
Once the learner performs an action, they must assess the outcome. That may require new orders or repeated testing, observational analysis, or patient and interdisciplinary communication.
It is entirely up to the learner to take control of the situation, effectively care for the patient, and communicate with their team.
After the scenario is concluded, learners are first required to complete a self-debrief, encouraging them to reflect on their experience prior to receiving any kind of feedback. The context of the scenarios themselves can also make for rich debriefing discussions, which are often conducted in small groups and facilitated by an experienced faculty member.
Feedback about how the learner led the scenario is automatically generated, providing time stamps of actions taken (or not taken), why those actions or concepts are important, and rationale is provided so learners can more deeply understand what went well and what needs to be improved.
Tags appear alongside feedback that can align with many different types of exams, and for the NGN, there is a tag for clinical judgment.
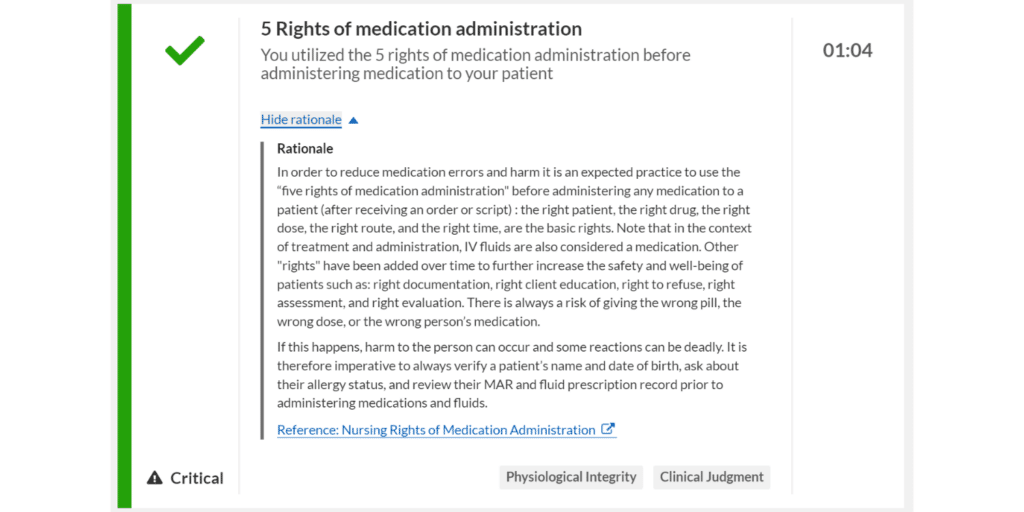
Learners can view which actions align with which pillars of the competency framework, providing clarity on what’s being assessed and how it all relates to practice.
The measurement of clinical judgment by the Next Generation NCLEX is truly an exciting time to be a part of nursing education and practice, and OMS is ready to support you and your learners as you prepare for the transition to practice.
To learn more about how OMS can support your learners, get in touch with us here.
